【协和医学杂志】欧洲抗风湿病联盟及美国风湿病学会关于IL-1介导的自身炎症性疾病诊疗指南解读
时间:2023-09-22 14:11:46 热度:37.1℃ 作者:网络
自身炎症性疾病(AIDs)主要是由固有免疫缺陷引起、累及多系统的一大类免疫失调性疾病[1]。其中,白细胞介素1(IL-1)在多种AIDs的发病机制中发挥重要作用,包括家族性地中海热(FMF)、冷炎素相关周期性综合征(CAPS)[又名NLRP3相关自身炎症性疾病(NLRP3-associated autoinflammatory diseases)]、肿瘤坏死因子受体相关周期性综合征(TRAPS)、甲羟戊酸激酶缺乏症(MKD)以及IL-1受体抑制剂缺陷(DIRA)等。
IL-1介导的AIDs通常由慢性全身性炎症和器官特异性炎症引起,并导致进行性器官损伤和功能障碍[2-5]。对于未经治疗的患者,病情急性发作时可危及生命,若病情持续活动可诱发多种并发症,死亡率较高[6-7]。
基于此,欧洲抗风湿病联盟(EULAR)及美国风湿病学会(ACR)成立了专门工作组,负责针对此类疾病的诊断、治疗、长期监测以及相关标准化指南的制定。2016年,EULAR发表了针对FMF的诊疗推荐意见[[8]];2022年,EULAR/ACR又共同发布了针对CAPS、TRAPS、MKD和DIRA的诊疗指南[9-10],旨在规范此类疾病的诊断、治疗和管理,提高患者的生活质量。本文针对该指南相关要点,结合中国人群特点进行详细解读,以期指导临床实践。
1 如何诊断CAPS、TRAPS、MKD和DIRA?
该指南指出,CAPS、TRAPS、MKD和DIRA的诊断均应结合临床表现和基因检测结果。
1.1 临床表现
1.1.1 CAPS
CAPS患者表现为全身炎症和荨麻疹样皮疹(病理表现为嗜中性粒细胞性皮病)。轻度患者可观察到寒冷诱发的疾病活动(通常持续不超过24 h);中/重度患者常出现进行性加重的感音神经性耳聋;神经系统表现(慢性无菌性脑膜炎、颅内压升高、认知障碍)和骨骼异常(股骨远端过度生长、额部凸起)常见于重度患者;眼部受累程度不一,典型表现为结膜炎,但角膜炎、巩膜外层炎、前葡萄膜炎和/或后葡萄膜炎亦有报道[11]。
就中国人群而言,发热、神经系统受累表现更多见,眼部受累相对少见[12]。考虑诊断为CAPS的患者应接受裂隙灯检查和视网膜评估[13];对于怀疑存在神经系统受累的患者,可行头部MRI和腰椎穿刺评估是否存在颅内压升高、无菌性脑膜炎、耳蜗强化、脑萎缩或脑室扩大[14];此外,可通过MRI或X线评估是否存在骨骺过度生长[15]。
1.1.2 TRAPS
TRAPS患者发热一般持续7 d以上;有类似急腹症的腹痛和不同程度的胸痛,偶见睾丸疼痛;典型皮疹表现为游走性斑块,边界不清,伴有红肿热痛;眶周水肿和肌痛常在急性期发作的起始阶段出现[7]。
1.1.3 MKD
MKD患儿常在1岁以内起病,反复发热持续4~6 d;胃肠道症状包括严重腹痛伴呕吐和腹泻;伴有颈部淋巴结肿大、阿弗他口炎和皮疹(荨麻疹或斑丘疹)[16-17]。病史中存在接种疫苗引发的发热是提示MKD的重要线索。辅助检查方面,单纯依靠免疫球蛋白D水平升高对于诊断MKD的灵敏度和特异度较低,而疾病发作期尿甲羟戊酸盐水平升高对于诊断MKD更具特异性[18]。
1.1.4 DIRA
DIRA典型表现为早发性脓疱性皮疹、无菌性骨髓炎和指甲改变(脱甲病)[19]。尽管炎症标志物通常显著升高,但与CAPS、TRAPS和MKD患者相比,DIRA患者较少出现发热。对于怀疑DIRA的患者应行X线检查评估胸部及四肢骨骼受累程度,行CT或MRI检查评估脊柱受累情况;皮肤活检发现嗜中性粒细胞皮肤病及角层下脓疱高度提示DIRA可能。
1.2 基因检测
CAPS和TRAPS分别是NLRP3[20]和TNFRSF1A[21]基因功能获得性突变引起的常染色体显性遗传病,而MKD和DIRA分别是MVK[22]和IL1RN[23]基因功能丧失性突变引起的常染色体隐性遗传病。该指南推荐在条件允许的情况下,对于怀疑上述疾病的患者,均应采用二代测序方法检测基因突变情况。尤其对于CAPS和TRAPS此类可能存在体细胞突变的情况,需进行深度测序[24]。
对于MKD和DIRA而言,Sanger测序或二代测序均有可能无法检测到基因中较大的缺失突变,因此对于高度怀疑但初始测序结果阴性的患者,可考虑进行染色体微阵列分析[23]。对于携带致病意义不明变异的患者,其遗传分析仍是目前的难点,需结合功能验证或变异分析。因此,该指南推荐对于常规基因检测无法给出诊断的患者,建议转诊至有丰富AIDs诊治经验的中心作进一步分析。
2 如何治疗CAPS、TRAPS、MKD和DIRA?
该指南指出,临床一旦高度怀疑CAPS、TRAPS、MKD或DIRA,即可考虑行IL-1拮抗剂治疗,并通常需用药维持较长时间。用药期间,即使出现病毒感染(包括新型冠状病毒在内),不推荐调整治疗方案。
目前国际已上市的IL-1拮抗剂共有3种:阿那白滞素、利纳西普和卡那单抗。其中阿那白滞素为重组IL-1受体拮抗剂,半衰期较短,可同时抑制IL-1α及IL-1β的信号传导[25];利纳西普为重组融合蛋白,可结合IL-1α及IL-1β,半衰期相对较长[26];而卡那单抗为人源IL-1β单克隆抗体,半衰期较长[27]。
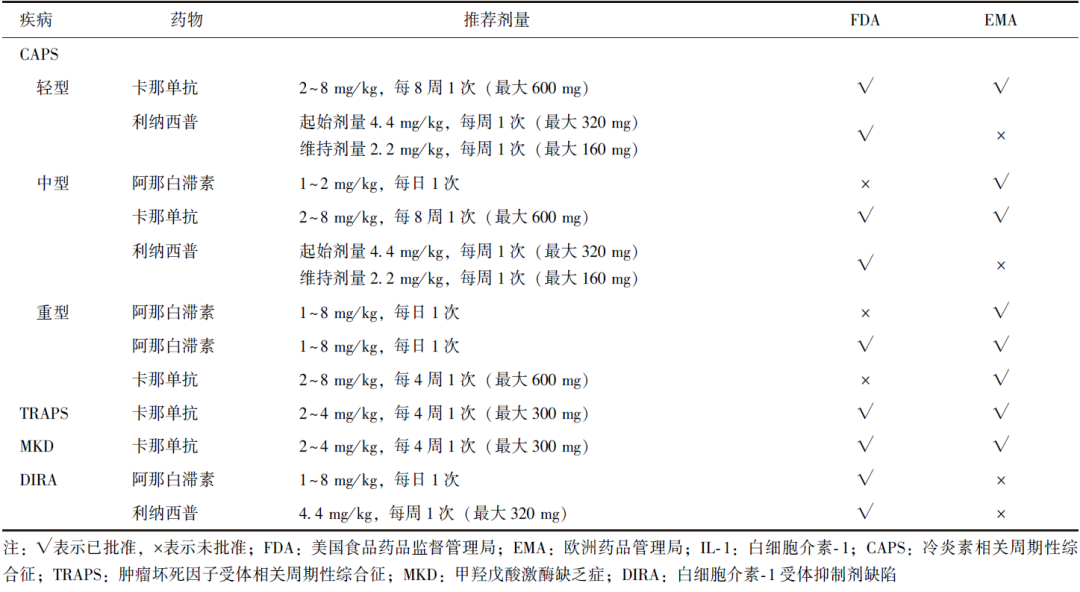
美国食品药品监督管理局(FDA)和欧洲药品管理局(EMA)已批准此3种药物用于某些情况下的CAPS、TRAPS、MKD和DIRA(表1)。
表1 FDA或EMA批准用于儿童IL-1相关自身炎症性疾病的IL-1拮抗剂及其用法
疗效评价方面,该指南将“完全缓解”定义为临床无症状且炎症指标正常。疾病活动度的评估可通过自身炎症性疾病活动指数(AIDAI)[28]、医师总体评估(PGA)和患者或家长总体评估(PPGA)进行。在治疗过程中,应根据年龄、治疗反应、体质量增长情况等个体化调整药物剂量。
对于婴儿及学龄前儿童,由于可能存在更多的肝脏代谢,阿那白滞素应根据个体情况增加给药剂量[29];对于病情严重的患者,可采用更大剂量更小间隔的治疗方案,而对于轻度CAPS、MKD及TRAPS,可考虑按需给药,即在疾病活动期用药,疾病间歇期停药[30-31];对于重度CAPS,尤其是存在神经系统表现的患者,阿那白滞素为首选用药[32];而对于DIRA患者,为同时阻断IL-1α及IL-1β,可选择阿那白滞素或利纳西普,但不推荐应用卡那单抗[33]。
除采用IL-1拮抗剂治疗外,对于急性期TRAPS,可短期应用糖皮质激素或益赛普治疗[34];IL-1拮抗剂治疗无效时,肿瘤坏死因子拮抗剂可作为MKD的二线治疗方案[30]。目前,IL-1拮抗剂尚未在我国批准上市,故对于MKD,多首选肿瘤坏死因子拮抗剂作为治疗方案,而对于其他疾病,多采用激素联合传统免疫抑制剂方案,此外也有应用托珠单抗、曲尼司特等药物治疗的报道,但整体疗效不如IL-1拮抗剂,在随访过程中发现患者易出现病情反复。
3 如何做好CAPS、TRAPS、MKD和DIRA的长期管理?
该指南指出,对于IL-1介导的AIDs患者的长期管理,需组建包括风湿免疫科、眼科、耳鼻喉科、肾内科、神经内科、遗传中心、物理康复治疗科、心理医学科等多学科专家在内的诊疗团队,在随访期间应考虑患者整个家庭的身心健康和社会功能。
在随访过程中,应注意根据年龄调整IL-1拮抗剂的剂量,以控制患者特异性炎症表现以及实验室指标。常用于评估IL-1介导的AIDs炎症标志物包括外周血中性粒细胞数目、C反应蛋白和红细胞沉降率,血清淀粉样蛋白A和S100蛋白也可用作标志物[35-36]。
持续的慢性炎症可能导致淀粉样变,因此推荐所有患者每半年行尿蛋白检测以筛查淀粉样变[27]。CAPS重点关注的器官损害包括听力下降、中枢神经系统异常、骨骼畸形、淀粉样变相关的肾衰竭以及视力损伤[6];对TRAPS而言,应着重关注是否存在不伴发热的持续炎症状态以及淀粉样变[5];MKD需警惕视网膜色素变性及听力下降的发生,以及感染后诱发巨噬细胞活化综合征的可能[37];DIRA主要关注点为炎症指标的控制情况及皮肤、骨骼病变的改善。
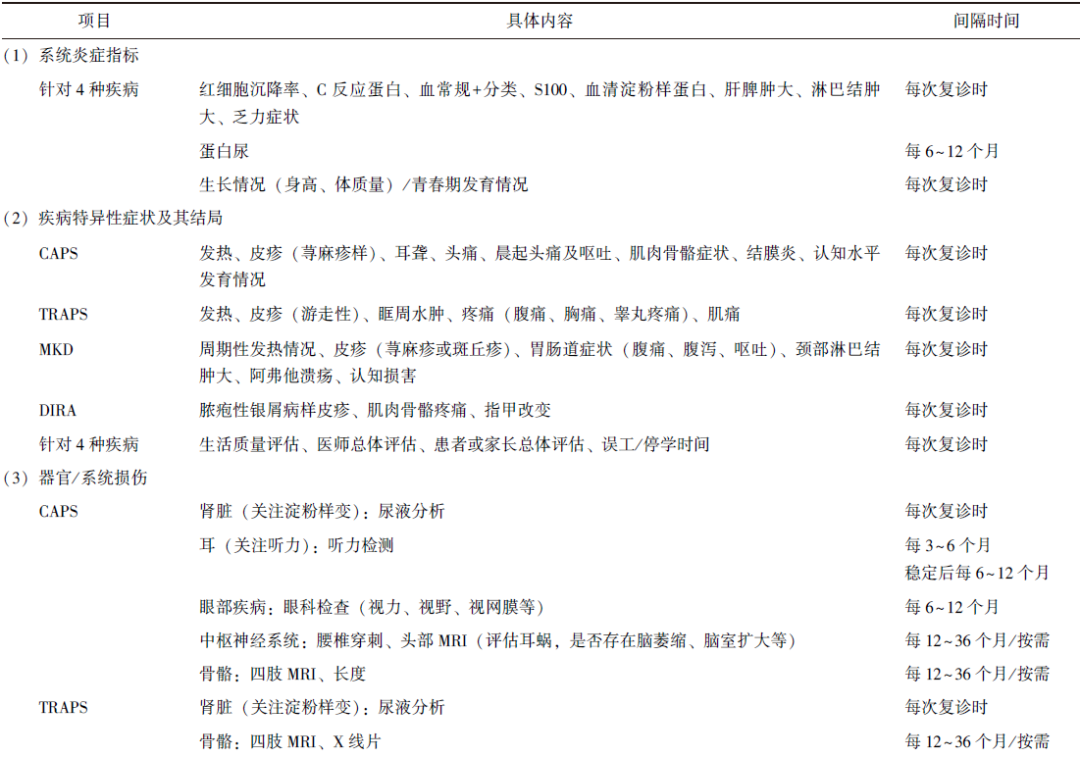
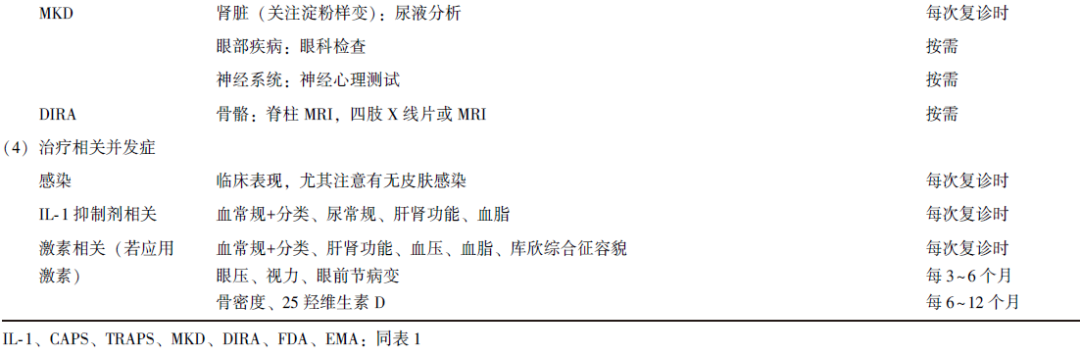
如前文所述,我国IL-1介导的AIDs应用IL-1拮抗剂治疗的比例低,激素用量更高,传统免疫抑制剂的使用更为普遍。因此我国患者在随诊过程中,应更关注激素相关的副作用。笔者根据指南原文结合我国国情整理了随诊推荐评估项目及其间隔时间,见表2。
表2 IL-1介导的自身炎症性疾病随诊推荐评估项目及其间隔时间
整体而言,IL-1拮抗剂治疗的安全性较高,但仍建议临床医生在随访过程中密切监测感染指标,特别应警惕肺炎链球菌引起的呼吸道感染和葡萄球菌引起的皮肤感染[38]。在条件允许的情况下,应在开始IL-1拮抗剂治疗前,按计划免疫程序接种疫苗,包括减毒活疫苗。目前有初步研究数据表明,即使在IL-1拮抗剂治疗中,患者接种疫苗后仍能产生足够的抗体反应[27]。由于专家组对于mRNA疫苗是否会引起疾病发作存在担忧,该指南未能就是否接种新型冠状病毒疫苗提出建议。
4 小结
依据近年来IL-1介导的AIDs领域的基础研究和临床试验结果,该指南提出了关于CAPS、TRAPS、MKD和DIRA的诊断、治疗、随访相关建议,为该类疾病的诊疗和长期管理提供了具体指导。但该指南在应用过程中仍然存在一定局限性,首先,受限于较低的疾病发病率,目前治疗方面的高质量随机对照研究较少,因此指南依据的文献主要来自于队列研究或个案报道,对于药物剂量及调整方案,有待于结合后续更多高质量研究结果进行更新;其次,随着诊疗技术的进步,患者的生存期将进一步延长,如何提高患者生活质量仍需更多的研究探索;再次,目前IL-1拮抗剂尚未在我国正式上市,国内人群对于IL-1拮抗剂治疗的安全性及有效性尚缺乏大样本研究。总之,临床医师应在该指南的指导下,结合我国国情及患者病情,制定个体化的治疗和随访方案。
参考文献
[1]Masters SL, Simon A, Aksentijevich I, et al. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease (*)[J]. Annu Rev Immunol, 2009, 27: 621-68.
[2]Ahmadi N, Brewer CC, Zalewski C, et al. Cryopyrin-associated periodic syndromes: otolaryngologic and audiologic manifestations[J]. Otolaryngol Head Neck Surg, 2011, 145: 295-302.
[3]Dollfus H, Hafner R, Hofmann HM, et al. Chronic infantile neurological cutaneous and articular/neonatal onset multisystem inflammatory disease syndrome: ocular manifestations in a recently recognized chronic inflammatory disease of childhood[J]. Arch Ophthalmol, 2000, 118: 1386-1392.
[4]Hill SC, Namde M, Dwyer A, et al. Arthropathy of neonatal onset multisystem inflammatory disease (NOMID/CINCA)[J]. Pediatr Radiol, 2007, 37: 145-152.
[5]Lane T, Loeffler JM, Rowczenio DM, et al. AA amyloidosis complicating the hereditary periodic fever syndromes[J]. Arthritis Rheum, 2013, 65: 1116-1121.
[6]Levy R, Gerard L, Kuemmerle-Deschner J, et al. Pheno-typic and genotypic characteristics of cryopyrin-associated periodic syndrome: a series of 136 patients from the Eurofever Registry[J]. Ann Rheum Dis, 2015, 74: 2043-2049.
[7]Lachmann HJ, Papa R, Gerhold K, et al. The phenotype of TNF receptor-associated autoinflammatory syndrome (TRAPS) at presentation: a series of 158 cases from the Eurofever/EUROTRAPS international registry[J]. Ann Rheum Dis, 2014, 73: 2160-2167.
[8]Ozen S, Demirkaya E, Erer B, et al. EULAR recommendations for the management of familial Mediterranean fever[J]. Ann Rheum Dis, 2016, 75: 644-651.
[9]Romano M, Arici ZS, Piskin D, et al. The 2021 EULAR/American College of Rheumatology points to consider for diagnosis, management and monitoring of the interleukin-1 mediated autoinflammatory diseases: cryopyrin-associated periodic syndromes, tumour necrosis factor receptor-associated periodic syndrome, mevalonate kinase deficiency, and deficiency of the interleukin-1 receptor antagonist[J]. Ann Rheum Dis, 2022, 81: 907-921.
[10]Romano M, Arici ZS, Piskin D, et al. The 2021 EULAR/American College of Rheumatology Points to Consider for Diagnosis, Management and Monitoring of the Interleukin-1 Mediated Autoinflammatory Diseases: Cryopyrin-Associated Periodic Syndromes, Tumour Necrosis Factor Receptor-Associated Periodic Syndrome, Mevalonate Kinase Deficiency, and Deficiency of the Interleukin-1 Receptor Antagonist[J]. Arthritis Rheumatol, 2022, 74: 1102-1121.
[11]Kuemmerle-Deschner JB, Ozen S, Tyrrell PN, et al. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS)[J]. Ann Rheum Dis, 2017, 76: 942-947.
[12]Zhou Y, Wang W, Zhong L, et al. Clinical and genetic spectrum of 14 cases of NLRP3-associated autoinflammatory disease (NLRP3-AID) in China and a review of the literature[J]. Orphanet J Rare Dis, 2022, 17: 214.
[13]Sobolewska B, Angermair E, Deuter C, et al. NLRP3 A439V Mutation in a Large Family with Cryopyrin-associated Periodic Syndrome: Description of Ophthalmologic Symptoms in Correlation with Other Organ Symptoms[J]. J Rheumatol, 2016, 43: 1101-1106.
[14]Kilic H, Sahin S, Duman C, et al. Spectrum of the neurologic manifestations in childhood-onset cryopyrin-associated periodic syndrome[J]. Eur J Paediatr Neurol, 2019, 23: 466-472.
[15]Li C, Tan X, Zhang J, et al. Gene mutations and clinical phenotypes in 15 Chinese children with cryopyrin-associated periodic syndrome (CAPS)[J]. Sci China Life Sci, 2017, 60: 1436-1444.
[16]Livneh A, Drenth JP, Klasen IS, et al. Familial Mediterranean fever and hyperimmunoglobulinemia D syndrome: two diseases with distinct clinical, serologic, and genetic features[J]. J Rheumatol, 1997, 24: 1558-1563.
[17]van der Hilst JCH, Bodar EJ, Barron KS, et al. Long-term follow-up, clinical features, and quality of life in a series of 103 patients with hyperimmunoglobulinemia D syndrome[J]. Medicine (Baltimore), 2008, 87: 301-310.
[18]Jeyaratnam J, Ter Haar NM, de Sain-van der Velden MG, et al. Diagnostic Value of Urinary Mevalonic Acid Excretion in Patients with a Clinical Suspicion of Mevalonate Kinase Deficiency (MKD)[J]. JIMD Rep, 2016, 27: 33-38.
[19]Garg M, de Jesus AA, Chapelle D, et al. Rilonacept maintains long-term inflammatory remission in patients with deficiency of the IL-1 receptor antagonist[J]. JCI Insight, 2017, 2: e94838.
[20]Feldmann J, Prieur AM, Quartier P, et al. Chronic infantile neurological cutaneous and articular syndrome is caused by mutations in CIAS1, a gene highly expressed in polymorphonuclear cells and chondrocytes[J]. Am J Hum Genet, 2002, 71: 198-203.
[21]Mcdermott MF, Aksentijevich I, Galon J, et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes[J]. Cell, 1999, 97: 133-144.
[22]D'osualdo A, Picco P, Caroli F, et al. MVK mutations and associated clinical features in Italian patients affected with autoinflammatory disorders and recurrent fever[J]. Eur J Hum Genet, 2005, 13: 314-320.
[23]Aksentijevich I, Masters SL, Ferguson PJ, et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist[J]. N Engl J Med, 2009, 360: 2426-2437.
[24]Rowczenio DM, Gomes SM, Arostegui JI, et al. Late-Onset Cryopyrin-Associated Periodic Syndromes Caused by Somatic NLRP3 Mosaicism-UK Single Center Experience[J]. Front Immunol, 2017, 8: 1410.
[25]Sibley CH, Plass N, Snow J, et al. Sustained response and prevention of damage progression in patients with neonatal-onset multisystem inflammatory disease treated with anak-inra: a cohort study to determine three- and five-year outcomes[J]. Arthritis Rheum, 2012, 64: 2375-2386.
[26]Hoffman HM, Throne ML, Amar NJ, et al. Long-term efficacy and safety profile of rilonacept in the treatment of cryopryin-associated periodic syndromes: results of a 72-week open-label extension study[J]. Clin Ther, 2012, 34: 2091-2103.
[27]Brogan PA, Hofer M, Kuemmerle-Deschner JB, et al. Rapid and Sustained Long-Term Efficacy and Safety of Canakinumab in Patients With Cryopyrin-Associated Periodic Syndrome Ages Five Years and Younger[J]. Arthritis Rheumatol, 2019, 71: 1955-1963.
[28]Piram M, Kone-Paut I, Lachmann HJ, et al. Validation of the auto-inflammatory diseases activity index (AIDAI) for hereditary recurrent fever syndromes[J]. Ann Rheum Dis, 2014, 73: 2168-2173.
[29]Batchelor HK, Marriott JF. Paediatric pharmacokinetics: key considerations[J]. Br J Clin Pharmacol, 2015, 79: 395-404.
[30]Bodar EJ, Kuijk LM, Drenth JP, et al. On-demand anakinra treatment is effective in mevalonate kinase deficiency[J]. Ann Rheum Dis, 2011, 70: 2155-2158.
[31]Grimwood C, Despert V, Jeru I, et al. On-demand treatment with anakinra: a treatment option for selected TRAPS patients [J]. Rheumatology (Oxford), 2015, 54: 1749-1751.
[32]Rodriguez-Smith J, Lin YC, Tsai WL, et al. Cerebrospinal Fluid Cytokines Correlate With Aseptic Meningitis and Blood-Brain Barrier Function in Neonatal-Onset Multisystem Inflammatory Disease: Central Nervous System Biomarkers in Neonatal-Onset Multisystem Inflammatory Disease Correlate With Central Nervous System Inflammation[J]. Arthritis Rheumatol, 2017, 69: 1325-1336.
[33]Kuemmerle-Deschner JB, Welzel T, Hoertnagel K, et al. New variant in the IL1RN-gene (DIRA) associated with late-onset, CRMO-like presentation[J]. Rheumatology (Oxford), 2020, 59: 3259-3263.
[34]Papa R, Lane T, Minden K, et al. INSAID Variant Classification and Eurofever Criteria Guide Optimal Treatment Strategy in Patients with TRAPS: Data from the Eurofever Registry[J]. J Allergy Clin Immunol Pract, 2021, 9: 783-991.e4.
[35]Ozen S, Kuemmerle-Deschner JB, Cimaz R, et al. International Retrospective Chart Review of Treatment Patterns in Severe Familial Mediterranean Fever, Tumor Necrosis Factor Receptor-Associated Periodic Syndrome, and Mevalonate Kinase Deficiency/Hyperimmunoglobulinemia D Syndrome[J]. Arthritis Care Res (Hoboken), 2017, 69: 578-586.
[36]Obici L, Meini A, Cattalini M, et al. Favourable and sustained response to anakinra in tumour necrosis factor receptor-associated periodic syndrome (TRAPS) with or without AA amyloidosis[J]. Ann Rheum Dis, 2011, 70: 1511-1512.
[37]Ter Haar NM, Jeyaratnam J, Lachmann HJ, et al. The Phenotype and Genotype of Mevalonate Kinase Deficiency: A Series of 114 Cases From the Eurofever Registry[J]. Arthritis Rheumatol, 2016, 68: 2795-2805.
[38]de Benedetti F, Gattorno M, Anton J, et al. Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes[J]. N Engl J Med, 2018, 378: 1908-1919.


