217项美国在研的癫痫基金简述,这两项课题的设计值得你借鉴(2024)
时间:2024-10-02 06:04:02 热度:37.1℃ 作者:网络
癫痫(Epilepsy)是一种中枢神经系统(神经元)的疾病,患者会经历突发的电活动异常,这些异常通常导致不同类型的癫痫发作。癫痫的发作可大致分为两大类:全身性发作和局部(局灶性)发作,且其症状范围可以从轻微的失神到剧烈的抽搐。
尽管近年来在癫痫的诊断和治疗方面取得了显著进展,但仍存在一些重要而未解决的临床问题:
-
治疗响应性差异:尽管有多种抗癫痫药物(AEDs)可用,但约30%的患者对现有药物治疗反应不佳,被称为难治性癫痫。这部分患者可能需要更复杂的治疗方案,包括手术或神经调控疗法。
-
诊断挑战:正确诊断癫痫类型对于选择合适的治疗方案至关重要,但在某些情况下,尤其是对于非典型发作或非发作性表现,诊断可能具有挑战性。
-
长期副作用:长期使用抗癫痫药物可能会带来副作用,如骨质疏松、肝脏问题和认知功能受损,管理这些副作用是治疗的一部分挑战。
-
生活质量影响:癫痫对患者的心理健康和生活质量有显著影响,患者可能面临就业困难、社交障碍和驾驶限制等问题。
-
意识和误解:社会对癫痫的误解仍然普遍,患者经常面临歧视和社会隔离。提高公众意识和改变公众对癫痫的态度是长期的社会挑战。
解决这些问题需要跨学科的合作,包括神经科学、药理学、心理学和社会科学的专家。持续的研究努力,旨在开发新的治疗方法、改善诊断工具和提高公众对癫痫的认知,对于提高患者的治疗效果和生活质量具有重要意义。
我们仅对美国国立卫生研究院(NIH)资助的在研癫痫相关项目进行梳理,希望给同仁们的选题思路提供一点启发。
2024年,以“Epilepsy”为检索词、在题目中进行检索,美国NIH针对癫痫的在研有217项。
一,谁获得了这些研究?
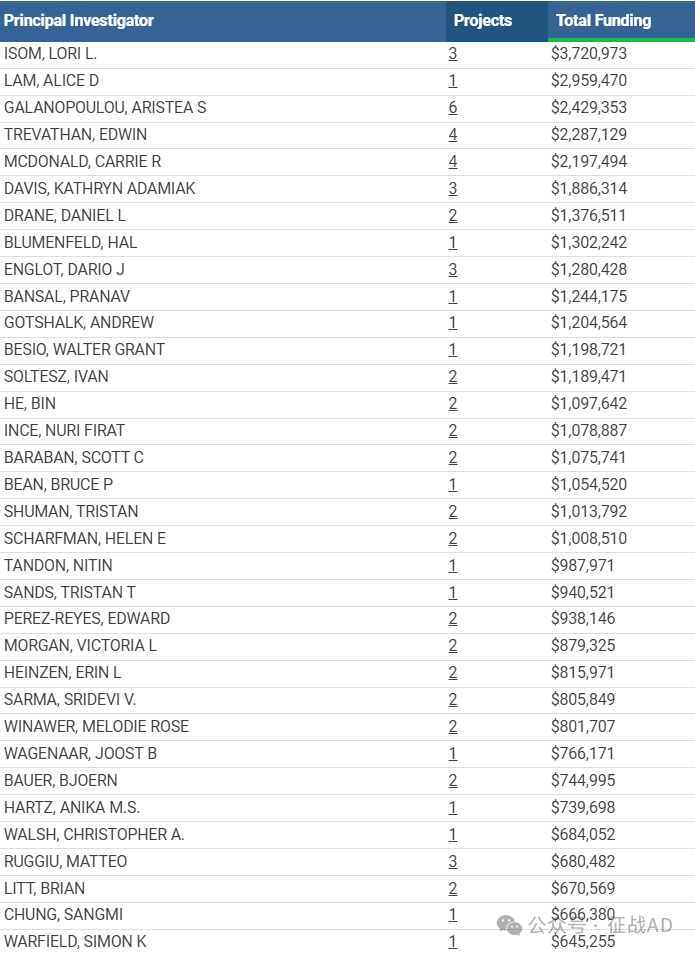
1,在研癫痫基金最多的PI
-
UNIVERSITY OF MICHIGAN AT ANN ARBOR 的 ISOM, LORI L.
-
MASSACHUSETTS GENERAL HOSPITAL 的 LAM, ALICE D
-
ALBERT EINSTEIN COLLEGE OF MEDICINE 的 GALANOPOULOU, ARISTEA S
-
VANDERBILT UNIVERSITY MEDICAL CENTER 的 TREVATHAN, EDWIN
-
UNIVERSITY OF CALIFORNIA, SAN DIEGO 的 MCDONALD, CARRIE R
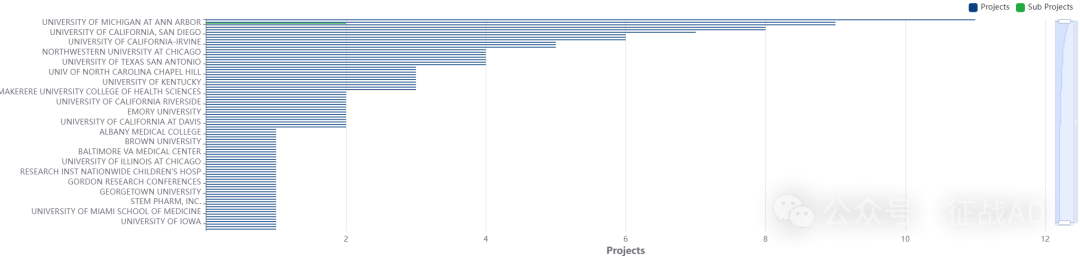
2,癫痫基金最多的研究机构
-
麻省总医院
-
范德堡大学医学中心
-
密歇根大学安娜堡分校
-
加州大学圣地亚哥分校
-
宾夕法尼亚大学等
二,癫痫研究热点是什么?
癫痫研究领域总览(根据关键词)

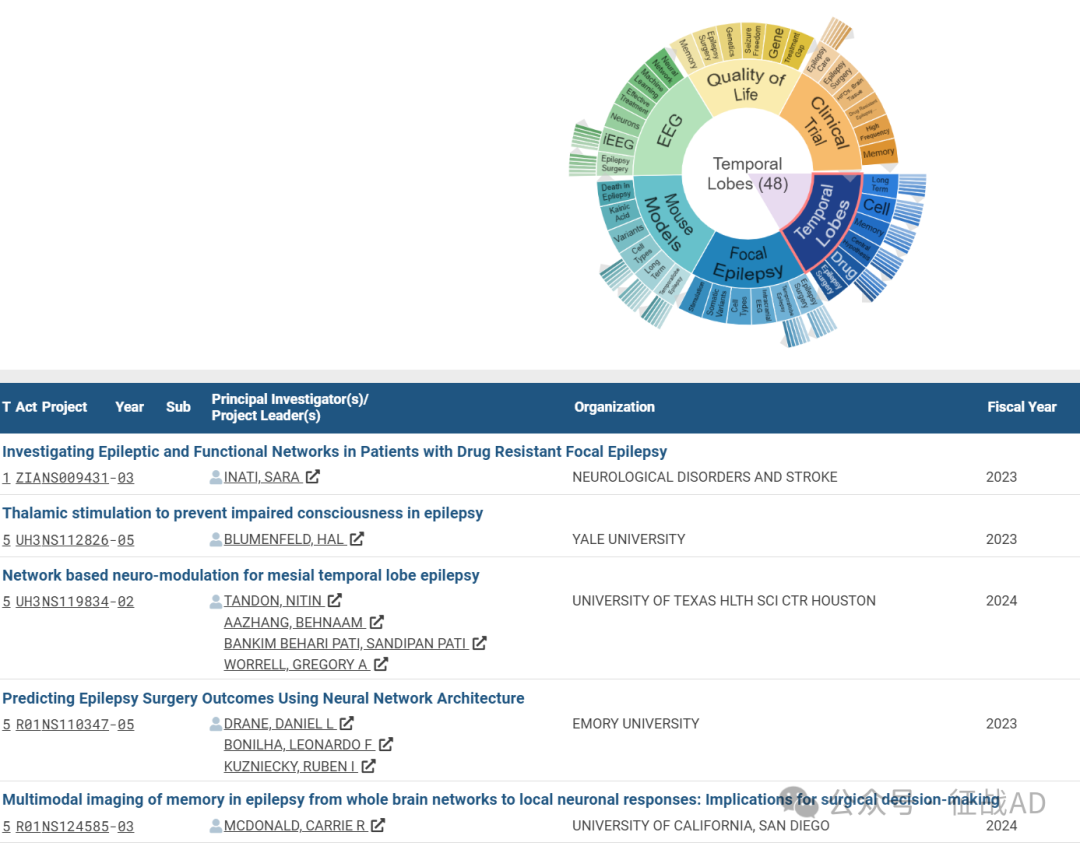
A,关于颞叶(Temporal Lobes)的研究项目最多
有 48 项在研基金涉及到了颞叶,关注最多的方面包括长期(Long Term)、细胞(Cell)、记忆(Memory)、中心假说(Central Hypothesis)、药物(Drug)、癫痫手术(Epilepsy Surgery)等研究。
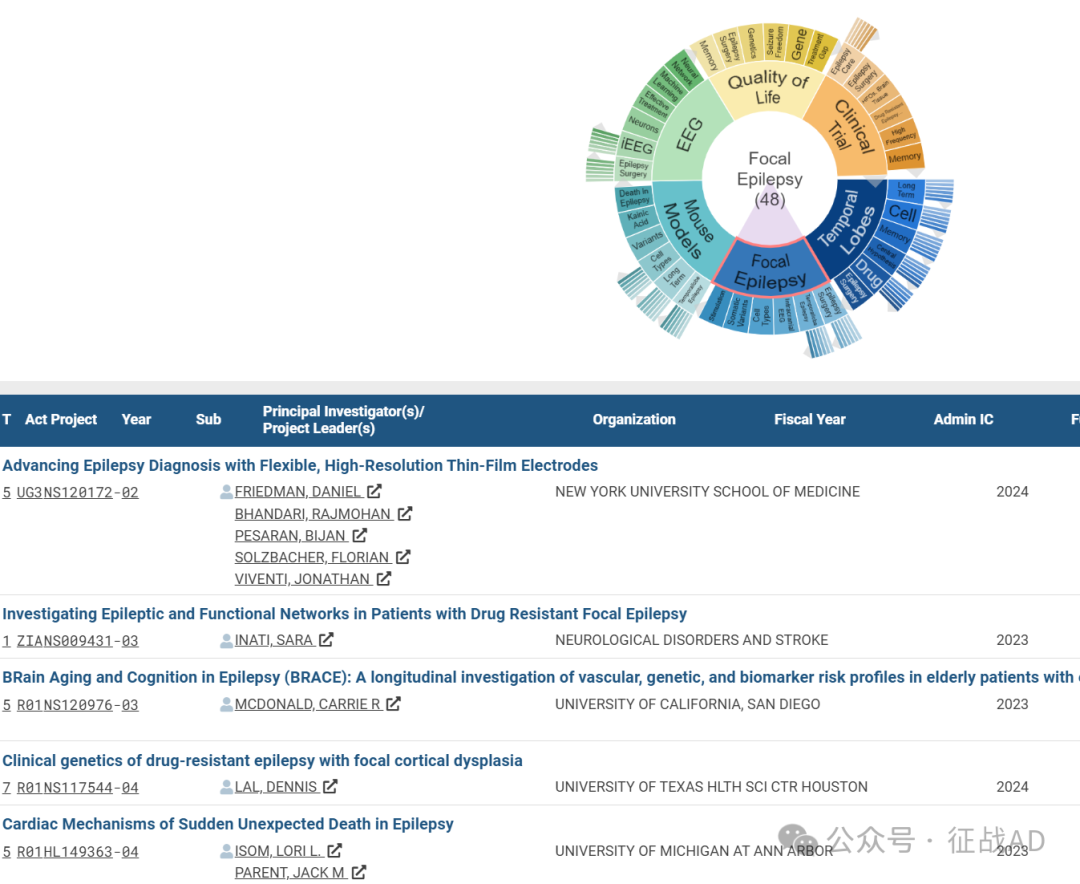
B,关于局灶性癫痫(Focal Epilepsy)的研究项目
有 48 项在研基金涉及到了局灶性癫痫,关注最多的方面包括癫痫手术(Epilepsy Surgery)、颞叶癫痫(Temporallobe Epilepsy)、颅内脑电图(Intracranial EEG)、细胞类型(Cell Types)、体细胞变异(Somatic Variants)、刺激(Stimulation)等研究。
C,关于小鼠模型(Mouse Models)的研究项目
有 46 项在研基金涉及到了小鼠模型,关注最多的方面包括颞叶癫痫(Temporallobe Epilepsy)、长期(Long Term)、细胞类型(Cell Types)、变异(Variants)、癫痫死亡(Death in Epilepsy)、红藻氨酸(Kainic Acid)等研究。

其他癫痫研究大的方向也包括EEG、生活质量(Quality of Life)、临床研究(Clinical Trail)等。
三,借鉴与突破
我们也分享在癫痫领域的几项课题摘要,希望对同仁们有所启发。
A,Epilepsy Multiplatform Variant Prediction (EpiMVP)
EpiMVP will develop a modular, highly integrated platform approach to accelerate determination of the functional, pharmacological, neuronal network and whole animal consequences of genetic variants implicated in a range of clinical epilepsy types. We will study non-ion-channel, non-receptor genes commonly implicated in epilepsy, and that are involved in diverse biological processes.
Our ultimate goals are to devise an effective experimental platform for testing the pathogenicity of VUS in genes implicated in epilepsy and to generate a computational model (EpiPred) that predicts the likelihood that a variant is pathogenic or benign. This work is crucial in the pursuit of novel therapeutics and the promise of personalized medicine.
The overall milestones of the Center are: 1. Evaluate genes associated with epilepsy and select candidates for analysis, model data for, and analyze all project data for development of EpiPred an iterative machine learning model to classify variants in genes implicated in epilepsy. 2. Test selected VUS using medium throughput, in vitro approaches. 3. Test selected VUS in human cortical neurons or human brain organoids using induced pluripotent stem cell approaches. 4. Test selected VUS in pre-clinical, in vivo models.
The expected outcomes are: 1. Provide a freely available prediction tool for clinicians to differentiate between pathogenic and benign variants for genes implicated in epilepsy; 2. Provide experimental models to study the functional consequences of specific variants; 3. Provide a reclassification of VUS in ClinVar/ClinGen and to develop new guidelines for incorporating functional readouts into the ACMG criteria; 4. Inform the future development of novel therapeutics to treat epilepsy.
B, A Phase 3 clinical trial of an e-health behavioral intervention to improve executive functioning in adolescents with epilepsy
To fill this gap, we successfully developed and tested Epilepsy Journey (EJ), a comprehensive e-health behavioral multi-component problem-solving intervention that combines 10 self-guided learning modules with 10 telehealth sessions. The promising proof-of-concept trial (n=39) showed high feasibility, acceptability, patient satisfaction, and significant improvements in parent-reported EF behaviors, neurobehavioral functioning, and quality of life.
The next logical phase of this research is to conduct a definitive randomized clinical trial to examine: 1) whether the two components of treatment (EJ modules and telehealth) are both essential, 2) if the intervention generalizes to a racially diverse sample, and 3) has a durable impact on improving parent-reported and performance-based EF behaviors. Thus, the aim of the current proposal is to conduct a multi-site Phase 3 randomized controlled clinical trial (RCT) using a 2x2 factorial design to examine the efficacy of separate (EJ modules and EJ telehealth) and combined components of EJ on EF.
Participants positive for EF deficits (n=232) will be randomized to one of four arms: 1) EJ modules with telehealth sessions, 2) EJ modules alone, 3) EJ telehealth sessions alone, or 4) Usual Care (no EJ modules or telehealth sessions). Treatment participants will either independently review EJ modules focused on EF skills (~15-30 min.) and/or have weekly telehealth sessions (~30-45 min.) with a therapist for three months. The groups will learn and apply problem-solving strategies to their individual EF difficulties. Participants will complete measures at baseline, post-treatment, 3- and 12-months post-treatment to examine maintenance of effects. There is a critical need for evidence-based interventions to improve executive functioning behaviors in youth with epilepsy. If the aims of this UG3/UH3 are achieved, we will have definitive evidence for addressing EF deficits. We expect that EJ modules and EJ telehealth will demonstrate efficacy alone and in combination, which will allow patients to select the approach best suited to their specific situation.


