【论著】| MMR蛋白在515例子宫内膜样腺癌中表达及其与临床病理学特征的相关性分析
时间:2023-08-24 17:44:22 热度:37.1℃ 作者:网络
[摘要] 背景与目的:林奇综合征(Lynch syndrome,LS)相关的子宫内膜癌有着独特的临床病理学特征及治疗手段。对新发子宫内膜癌患者采用免疫组织化学(immunohistochemistry,IHC)染色的方法检测错配修复(mismatch repair,MMR)蛋白表达情况,可以有效地筛查LS相关的癌症患者。本研究探讨MMR蛋白(MLH1、MSH2、MSH6及PMS2)在子宫内膜样腺癌中的表达情况及其与患者临床病理学特征的关系。方法:收集中国医科大学盛京医院2018年1月—2020年8月共515例子宫内膜样腺癌连续性病例为研究对象,年龄范围为28~81(57.73±8.41)岁。采用IHC染色的方法检测癌组织中MLH1、MSH2、MSH6和PMS2蛋白表达情况,应用聚合酶链式反应(polymerase chain reaction,PCR)方法对MLH1蛋白表达缺失的标本进行基因的甲基化检测,并且分析MMR蛋白表达缺失情况与子宫内膜样腺癌临床病理学特征的关系。只要有一种MMR蛋白表达缺失即判定为MMR蛋白错配修复缺陷(deficient mismatch repair,dMMR),蛋白全部阳性则判定为MMR表达完整(proficient mismatch repair,pMMR)。结果:515例子宫内膜样腺癌中有138例(26.8%)发生MMR蛋白表达缺失,MLH1、PMS2、MSH2及MSH6蛋白表达缺失率分别是16.3%(84/515)、19.0%(98/515)、5.4%(28/515)、 8.0%(41/515)。MMR蛋白的缺失以MLH1和PMS2联合表达缺失(60.9%,84/138)为主;其次为MSH2和MSH6联合表达缺失(18.8%,26/138);MSH2、MSH6和PMS2联合表达缺失有2例(1.4%,2/138);PMS2、MSH2和MSH6蛋白单独表达缺失比例分别为8.0%(11/138)、1.4%(2/138)、10.1%(14/138)。对27例MLH1蛋白表达缺失标本进行甲基化检测,结果显示,阳性率为85.2%(23/27)。515例子宫内膜样腺癌组织中的MMR蛋白表达缺失与患者发病年龄、国际妇产科联合会(The International Federation of Gynecology and Obstetrics,FIGO)分期、组织学分化程度、浸润深度、脉管转移、神经侵犯、淋巴结转移、p53异常表达、肿瘤浸润淋巴细胞(tumor infiltrating lymphocyte,TIL)及肿瘤伴瘤周淋巴细胞有相关性,而与是否累及子宫下段无关。与pMMR的患者相比,dMMR的患者发病年龄更小,FIGO临床分期多为Ⅲ~Ⅳ期,组织学分化程度多为低分化,肿瘤多无肌层浸润,肿瘤多出现脉管神经侵犯及淋巴结转移,肿瘤浸润淋巴细胞增多,且肿瘤伴瘤周淋巴细胞更显著,MSH6蛋白缺失患者多无p53异常表达。结论:dMMR的子宫内膜样腺癌患者具有独特的临床病理学特征。应用免疫组织化学染色方法检测MMR蛋白表达情况,并对MLH1表达缺失的标本进行基因甲基化检测,能初步筛查LS患者,对肿瘤患者免疫治疗具有一定指导意义。
[关键词] 子宫内膜样腺癌;错配修复缺陷;微卫星不稳定性;免疫组织化学;免疫治疗
[Abstract]Background and purpose: Lynch syndrome associated endometrial carcinoma has unique clinicopathological features and treatment methods. The detection of mismatch repair (MMR) protein expression by immunohistochemical (IHC) staining in patients with newly diagnosed endometrial cancer can effectively screen patients with Lynch syndrome associated cancer. This study investigated the expression of mismatch repair proteins (MLH1, MSH2, MSH6 and PMS2) in endometrioid adenocarcinoma and its relationship with clinicopathological features. Methods: A total of 515 cases of endometrioid adenocarcinoma were collected from Shengjing Hospital of China Medical University from January 2018 to August 2020.The patients were 28 to 81 (57.73 ± 8.41) years old. IHC method was used to detect the protein expressions of MLH1, MSH2, MSH6 and PMS2 in cancer tissues. Polymerase chain reaction (PCR) was used to detect the gene methylation of MLH1 protein expression deficient specimens, and the relationship between MMR protein expression deletion and clinicopathological features of endometrioid adenocarcinoma was analyzed. As long as there was a loss of MMR protein expression, it was judged as deficient mismatch repair (dMMR). If all MMR proteins were positive, it was judged as proficient mismatch repair (pMMR). Results: MMR protein was absent in 138 (26.8%) of 515 cases of endometrioid adenocarcinoma. The deletion rates of MLH1, PMS2, MSH2 and MSH6 proteins were 16.3% (84/515), 19.0% (98/515), 5.4% (28/515) and 8.0% (41/515), respectively. The loss of MMR protein expression was mainly the combined loss of MLH1 and PMS2 expressions (60.9%, 84/138), and the second was the combined deletion of MSH2 and MSH6 expressions (18.8%, 26/138). There were 2 cases of combined deletion of MSH2, MSH6 and PMS2 expressions (1.4%, 2/138). The single deletion rates of PMS2, MSH2 and MSH6 proteins were 8.0% (11/138), 1.4% (2/138) and 10.1% (14/138), respectively. MLH1 protein expression deletion was detected in 27 samples, and the results showed that the methylation positive rate was 85.2% (23/27). The loss of MMR protein expression in 515 cases of endometrioid adenocarcinoma was correlated with the age of onset, the International Federation of Gynecology and Obstetrics (FIGO) stage, the degree of histological differentiation, depth of invasion, vascular metastasis, nerve invasion, lymph node metastasis, abnormal expression of p53, tumor infiltrating lymphocytes and tumor with peritumoral lymphocyte infiltration. MMR protein status was not correlated with lower uterine segment involvement. Compared with pMMR patients, the onset age of dMMR was younger, and FIGO stage was mostly stage Ⅲ-Ⅳ. The histological differentiation degree was mostly low, most tumors had no myometrial infiltration, and most tumors had vascular metastasis, nerve invasion and lymph node metastasis. The lymphocyte infiltration in the tumor with dMMR was increased, and the tumor with peritumoral lymphocyte was more significant. Most patients with MSH6 protein deficiency had no abnormal expression of p53. Conclusion: Compared with pMMR patients, dMMR patients in Northeast China has unique clinicopathological characteristics. Detecting the expression of MMR protein by immunohistochemical staining and detection of the gene methylation of MLH1 expression deficient specimens can preliminarily screen patients with Lynch syndrome, which has certain guiding significance for immunotherapy of tumor patients.
[Key words] Endometrioid adenocarcinoma; Deficient mismatch repair; Microsatellite instability; Immunohistochemistry; Immunotherapy
子宫内膜癌的发病率呈逐年上升趋势,其最常见的组织学亚型是子宫内膜样腺癌,约占新诊断病例的85%[1]。林奇综合征(Lynch syndrome,LS)是由DNA错配修复(mismatch repair,MMR)基因突变引起的一种常染色体显性遗传性疾病,是常见的癌症易感综合征之一,其特点是能够增加癌症患病风险,其中以结直肠癌和子宫内膜癌最为多见[2]。患有LS的女性一生中患子宫内膜癌的风险为40%~60%[3]。
MMR系统能够通过识别并纠正DNA复制过程中产生的错误配对,修复DNA损伤,来维持基因组的稳定性。DNA错配修复缺陷(deficient mismatch repair,dMMR)可导致一种强突变表型,称为微卫星不稳定性(microsatellite instability,MSI),这种分子变化特点是会导致大多数LS的发生,是LS患者肿瘤的典型分子变化[4]。因此,dMMR和MSI的识别非常重要,因为这是LS相关癌症的重要标志,可以作为检测LS的筛选工具[5]。
目前,国内针对LS相关的子宫内膜癌的研究仍处于起步阶段,且多数研究数据来自欧美国家,其临床病理学特征是否适合中国国民,仍有待考证。本研究使用特异性抗体,通过免疫组织化学(immunohistochemistry,IHC)染色方法,对515例子宫内膜样腺癌患者进行MMR蛋白缺失的检测,当出现 MLH1、PMS2、MSH2及 MSH6蛋白中的一个及多个蛋白表达缺失时,则初步诊断为LS相关子宫内膜样腺癌;造成MLHI蛋白表达缺失的原因除MLH1基因胚系突变外,还包括MLH1基因甲基化导致的MLH1基因沉默。因此,对MLH1蛋白表达缺失患者,需进一步检测癌组织中MLH1基因的甲基化情况,若MLH1基因甲基化阳性,则可排除LS相关子宫内膜样腺癌,而为散发性子宫内膜样腺癌。本研究旨在探讨MMR蛋白在子宫内膜样腺癌中的表达情况及其与患者临床病理学特征之间的关系,并为加强LS相关的子宫内膜样腺癌人群筛查提供依据。
1 资料和方法
1.1 临床资料来源
收集中国医科大学附属盛京医院2018年1月—2020年8月收治的经手术切除全子宫的子宫内膜样腺癌病例,未经人为干预随意删除病例,只要患者有完整的临床数据及病理学报告数据,均纳入了本研究。患者临床病历资料完整且有相应的切片及石蜡包埋标本可用于实验。通过复阅相关病例的H-E切片及本院诊断系统诊断结果,统计患者发病年龄、肿瘤分化程度、国际妇产科联合会(The International Federation of Gynecology and Obstetrics,FIGO)分期、p53有无异常表达、浸润深度、有无淋巴结转移、有无脉管癌栓及神经侵犯、是否累子宫下段等临床病理学特征。本研究通过中国医科大学附属盛京医院伦理委员会批准。通过MMR蛋白IHC染色及MLH1基因甲基化的检测结果,初步诊断LS相关子宫内膜样腺癌患者,分析其发病特点及临床病理学特 征。
1.2 IHC染色方法及结果判读
通过全自动IHC染色系统(生产厂家为Ventana Medical Systems,Inc),采用IHC法检测515例子宫内膜样腺癌患者肿瘤组织MMR蛋白(MLH1、MSH2、MSH6和PMS2)的表达情况。首先用3.7%的甲醛液对标本进行固定,由本院病理科医师取材,随后依次进行脱水、石蜡包埋,切片(厚度为3~4 μm),切片行常规H-E染色及IHC染色(包括修复抗原、滴加抗体、磷酸盐缓冲液冲洗、DAB显色、苏木精复染、盐酸乙醇分化等处理),一抗分别采用鼠抗人单克隆抗体MLH1(M1)、兔抗人单克隆抗体MSH6 (SP93)、鼠抗人单克隆抗体MSH2(G219-1129)及鼠抗人单克隆抗体PMS2(A16-4)。抗体均购自上海罗氏制药有限公司。以切片内非肿瘤细胞核着色阳性为内对照,用磷酸盐缓冲生理盐水(phosphate-buffered asline,PBS)代替一抗作为空白对照。若MMR蛋白在肿瘤细胞核明确着棕褐色即判定为阳性,不论任何比率的肿瘤细胞呈阳性,且与染色强弱以及阳性细胞弥漫或局灶分布无关。肿瘤细胞核不着色判断为阴性。p53定位于细胞核,其阳性信号呈棕黄色或棕褐色颗粒。随机选择10个高倍镜视野,计数其中阳性癌细胞的比率:p53呈现弥漫阳性(>70%)或完全阴性时,均判定为p53突变型,否则为p53野生型。
1.3 MLH1基因甲基化的检测
对84例MLH1缺失的患者中的27例标本进行甲基化检测,采用焦磷酸测序技术,实验步骤按照说明书进行。PCR反应扩增仪购自美国ABI公司(反应条件为 95℃ 3 min,95℃ 15 s,54℃20 s,72℃ 30 s,50次循环,72℃ 5 min),焦磷酸序列分析仪购自德国QIAGEN公司。将测序反应板置于PyroMark Q96序列分析仪中,采用配套软件Q96 CpG Software分析目标基因位点的甲基化状态。检测区段共包含5个CpG位点,最终结果取5个位点平均值,正常人全血DNA的MLH1基因甲基化检测结果≤6%,若>6%,即判定为MLH1基因甲基化阳性。若检测结果为MLH1基因甲基化阳性,则提示该病例为散发性子宫内膜样腺癌,而非LS相关的子宫内膜样腺癌。
1.4 肿瘤浸润淋巴细胞及肿瘤伴瘤周淋巴细胞
肿瘤浸润淋巴细胞(tumor infiltrating lymphocyte,TIL)定义:位于肿瘤细胞巢或腺体边界内的淋巴细胞(不包括肿瘤间质内的淋巴细胞和凋亡小体)。评判标准为每10个高倍镜下(淋巴细胞数量最高的区域进行计数)淋巴细胞 ≥42个(图2A),肿瘤伴瘤周淋巴细胞定义:显微镜放大可见瘤周有明显的淋巴细胞聚集[6](图2B、C)。
1.5 统计学处理
应用SPSS 26.0软件进行统计学分析。计数资料的组间比较采用卡方检验。P<0.05为差异有统计学意义。
2 结 果
2.1 515例子宫内膜样腺癌MMR蛋白及p53蛋白的表达情况
515例子宫内膜样腺癌MMR蛋白及p53蛋白IHC染色结果显示,阳性表达着色于细胞核,可伴有细胞质弱阳性。本组515例患者中有138例(26.8%)发生了MMR蛋白表达缺失,MLH1、PMS2、MSH2及MSH6蛋白表达缺失率分别是16.3%(84/515)、19.0%(98/515)、 5.4%(28/515)和8.0%(41/515),其中以MLH1和PMS2联合表达缺失(60.9%,84/138)为主;其次为MSH2和MSH6联合表达缺失(18.8%,26/138);MSH2、MSH6和PMS2联合表达缺失的有2例(1.4%,2/138);PMS2、MSH2和MSH6蛋白表达单独缺失的比例分别为8.0%(11/138)、1.4%(2/138)、10.1%(14/138)。MMR蛋白及p53蛋白表达模式见图1。
2.2 MLH1蛋白缺失的患者MLH1基因甲基化检测结果
对84例MLH1缺失的患者中的27例标本进行甲基化检测,结果显示甲基化阳性率为85.2%(23/27),提示该23例患者可能存在因基因甲基化而导致的MLH1蛋白表达缺失,为散发型患者(图3)。
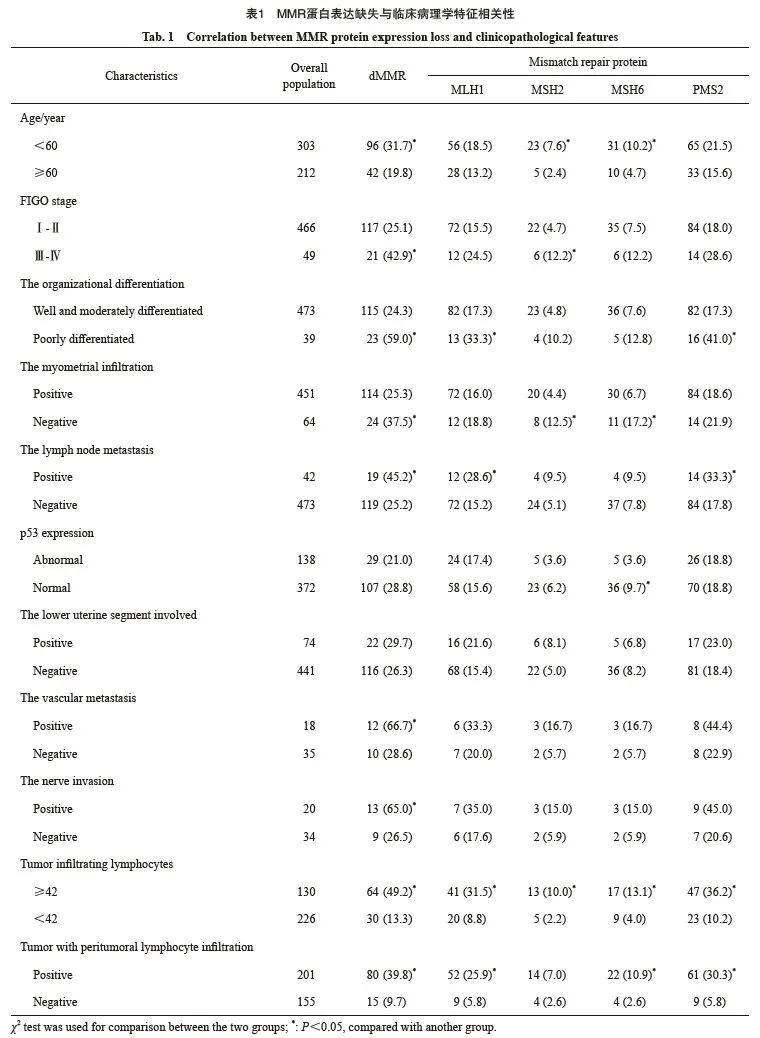
2.3 MMR蛋白表达缺失情况与临床病理学特征的相关性分析
515例子宫内膜样腺癌组织中的MMR蛋白的表达缺失与患者发病年龄、FIGO分期、组织学分化程度、浸润深度、脉管转移、淋巴结转移、p53异常表达、肿瘤浸润淋巴细胞及肿瘤伴瘤周淋巴细胞有关(P<0.05),而与是否累及子宫下段无相关性(P>0.05)。与pMMR的子宫内膜样腺癌患者相比,dMMR患者的发病年龄更小,FIGO临床分期多为Ⅲ~Ⅳ期,组织学分化程度多为低分化,肿瘤多无肌层浸润,患者多出现脉管、神经侵犯及淋巴结转移,肿瘤浸润淋巴细胞增多,且肿瘤伴瘤周淋巴细胞更显著,MSH6蛋白缺失患者多无p53异常表达。具体情况见表1。
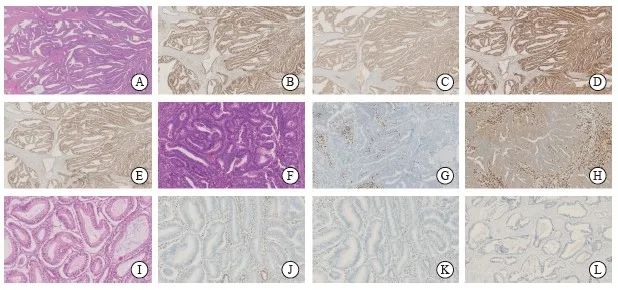
图1 子宫内膜样腺癌中MMR蛋白及p53蛋白的表达
Fig. 1 The expression of MMR protein and p53 protein in endometrioid adenocarcinoma
A-E: H-E and IHC staining in the same case of endometrial cancer (×25); A: H-E staining of well differentiated endometrioid adenocarcinoma; B: MLH1 protein was positively expressed in tumor nuclei; C: PMS2 protein was positively expressed in tumor nuclei; D: MSH2 protein was positively expressed in tumor nuclei; E: MSH6 protein was positively expressed in tumor nuclei. F-H: H-E and IHC staining in the same case of endometrial cancer (×100); F: H-E staining of moderately differentiated endometrioid adenocarcinoma; G: The expression of MLH1 protein was negative in tumor nucleus and positive in interstitial nucleus; H: The expression of PMS2 protein was negative in tumor nucleus, weakly positive in tumor cell membrane and positive in interstitial nucleus. I-L: H-E and IHC staining in the same case of endometrial cancer (×100); I: H-E staining of well differentiated endometrioid adenocarcinoma; J: The expression of MSH2 protein was negative in tumor nucleus; K: The expression of MSH6 protein was negative in tumor nucleus and positive in interstitial nucleus; L: Abnormal expression of p53 protein, the expression of p53 protein was negative in tumor nucleus.
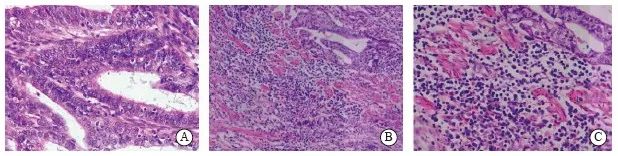
图2 肿瘤浸润淋巴细胞及肿瘤伴瘤周淋巴细胞
Fig. 2 Tumor infiltrating lymphocytes and tumor with peritumoral lymphocytes
A. Tumor infiltrating lymphocytes (×400); B: Peritumoral lymphocytes (×200); C: Peritumoral lymphocytes (×400).
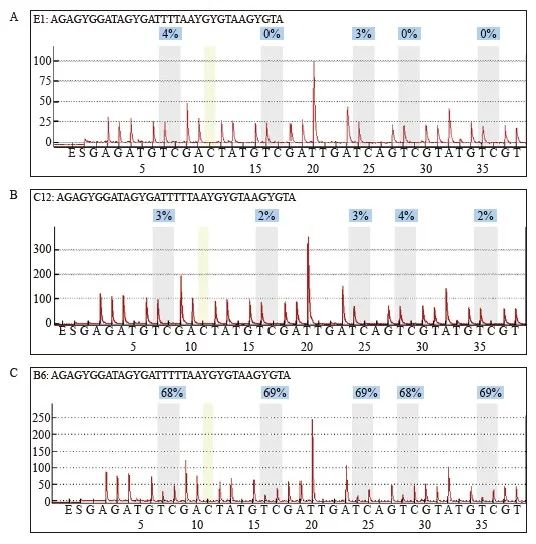
图3 MLH1蛋白表达缺失子宫内膜样腺癌中MLH1甲基化检测结果
Fig. 3 MLH1 methylation was detected in sample with protein expression deletion
A: Reference map of normal samples; B:MLH1 methylation was negative in dMMR endometrioid adenocarcinoma with MLH1 protein expression deletion; C: MLH1 methylation was positive in dMMR endometrioid adenocarcinoma with MLH1 protein expression deletion.
3 讨 论
MMR系统主要包括MLH1、PMS2、MSH2和MSH6,能够识别并纠正DNA错配,修复DNA损伤,维持基因组的稳定性[4]。微卫星是包含1~4个碱基对的短串联重复DNA序列,由于其重复结构,很容易发生复制错误,通常由MMR系统修复。MMR基因突变导致的dMMR可产生一种强突变表型,即MSI,MSI是发生在LS患者中的肿瘤典型的分子变化,其特征是简单重复微卫星序列的长度变化[5],MSI会导致大多数LS的发生,与普通人群相比,LS患者的各种癌症患病风险显著增加,因此,筛查新发病例中的LS患者至关重要[7]。LS最根本的诊断依据是遗传学基因突变检测,然而,在实际临床工作中,由于突变检测价格昂贵、检测费时等,临床普及较困难。据研究统计,相较于基因检测,利用IHC检测具体蛋白表达缺失,提示某一个或者多个MMR基因突变的敏感性和特异性较高,为初步筛选LS患者的有效方法[8-9] 。因此,本研究旨在通过IHC的方法探究MMR缺失与患者临床病理学特征的相关性,为子宫内膜癌的精准治疗和预后预测提供新的启示和理论基础。
关于dMMR的发生频率已有多项研究,其数据各不相同,这可能与各研究中收集的标本类型不同或地域差别有关。本研究中共有138例(26.8%)发生MMR蛋白表达缺失。低于Manchana等[10]报道的34.9%、晋薇等[11]报道的34.5%和Zhao等[12]报道的29.89%,高于文献[13]报道的21.6%。本研究结果显示,MMR蛋白表达缺失以MLH1和PMS2联合表达缺失为主;其次为MSH2和MSH6联合表达缺失;这与研究[10-11,14]报道的结果相同。MMR蛋白表达缺失率由高到低排序依次为PMS2、MLH1、MSH6、 MSH2(缺失率分别为19.0%、16.3%、8.0%、 5.4%)。其中PMS2缺失率最高,MSH6与MSH2的缺失率差异不显著,这与晋薇等[11]报道的数据基本一致。值得注意的是,尽管MLH1基因缺失率较高,但其中不乏MLH1基因甲基化的患者,需进一步对标本进行MLH1基因甲基化检测。
目前,子宫内膜癌发生平均年龄约为60岁,但LS相关的子宫内膜癌患者诊断时的平均年龄小于散发型患者[12]。此外,有研究[13]表明,不同突变体的发病年龄也不同:与MSH2或MLH1突变相比,MSH6突变者出现子宫内膜癌的年龄较晚,MSH6基因突变者子宫内膜癌发病年龄为50.6~59.5岁,而MLH1和MSH2基因突变患者发病年龄为39.0~49.5岁,本研究结果显示,与pMMR的子宫内膜样腺癌患者相比,dMMR患者发病年龄更小,究其原因,MMR缺失可能会使患者发病年龄提前,这将为制定个体化预防措施提供理论依据。另有研究[11]显示,dMMR患者肿瘤组织更易浸润深肌层,这与本研究结果(dMMR肿瘤患者肿瘤组织多无肌层浸润)相悖,也有研究[14]表明错配修复蛋白缺失的患者肿瘤浸润深度通常小于1/2肌层,分析其原因,可能是由于不同研究人员临床病理学数据和纳入标准存在主观差异、样本量不同以及地域差异,因此,需要扩大病例数深入研究。
关于LS相关的FIGO临床分期特征仍存在争议。本研究结果显示,dMMR患者FIGO分期Ⅲ~Ⅳ期更多见,呈现较高的临床分期,且组织学分化程度多为低分化,提示预后不良。McMeekin等[15]认为MMR缺陷与预示不良预后的临床特征(较高的肿瘤级别、淋巴血管间隙侵犯的存在及淋巴结转移比例高)显著相关,这与本研究MMR缺陷患者组织学分化程度多为低分化,多出现脉管、神经侵犯及淋巴结转移相似。综上所述,就纳入本研究的515例子宫内膜样腺癌患者而言,其中MMR蛋白缺失的患者表现出独特的临床病理学特征,可推测MMR缺陷与预后不良的临床特征(较高的肿瘤临床FIGO分期、组织学分化程度多为低分化、脉管转移及神经侵犯及淋巴结转移)相关,提示MMR蛋白缺失可能导致预后不良。另外,肿瘤浸润淋巴细胞与患者临床预后相关:一方面,肿瘤浸润淋巴细胞可抑制肿瘤的生长和进展;另一方面,又可促进免疫抑制而帮助肿瘤细胞免疫逃逸,其最终发挥的效应,是其各个亚群在肿瘤免疫微环境中相互平衡博弈的结果[16]。McMeekin[15]和Shikama等[17]指出,尽管dMMR的患者临床分期更高,淋巴血管间隙侵犯更多,但却与良好的总体生存结局相关。他们认为,MMR缺陷可能会抵消以上不良预后的影响。本研究结果表明,肿瘤浸润淋巴细胞及肿瘤伴瘤周淋巴细胞在dMMR组中明显高于pMMR组,因此,我们推测这可能将成为改善患者预后的因素。
研究[15]表明,MMR缺失的结直肠癌患者生存期有改善,但dMMR对子宫内膜癌的预后影响尚无确切定论,也有研究[17]表明dMMR与患者不良预后相关或无差异,看来还需更多大规模的研究。另外,多数子宫内膜样腺癌发现时为早期阶段(FIGO分期Ⅰ或Ⅱ),因此,子宫内膜样腺癌患者复发的绝对风险很低,5年总生存率接近90%[18]。我们随访了515例患者,有49例失访,仅有19例死亡,其中因子宫内膜样腺癌复发死亡的有15例,因此针对dMMR患者对子宫内膜样腺癌预后的影响还需要更长的随访时间才能得出结论,这也是本研究未来的方向之一。
2013年美国癌症基因组图谱(the Cancer Genome Atlas,TCGA)项目将子宫内膜癌划分为4种分子亚型:POLE突变型、微卫星不稳定型、低拷贝数型和高拷贝数型[19]。研究证实,不同分子特征可能导致辅助放化疗敏感性差异,如p53基因突变型患者接受放化疗比单纯放疗的5年无复发生存率明显增高[20],因此,TCGA分子分型能更准确地指导子宫内膜癌患者术后治疗及预测预后。TP53基因作为一种抑癌基因,涉及许多DNA修复机制,p53蛋白失活或异常与肿瘤的发生、发展相关。研究[21]表明,p53和MMR之间的关系似乎集中在MMR核心组分MSH2上。Cranston等[22]的研究显示,p53和MMR在小鼠中协同发挥作用。另外,在体外,Subramanian等[23]证实MSH2~MSH6复合物可以通过拓扑畸变增强p53与DNA底物的结合。目前鲜有关于MMR蛋白与p53蛋白表达的相关性研究,本研究结果表明,MSH6蛋白缺失患者多无p53异常表达,该结论仍需进一步深入研究。
研究表明,MMR表达缺失可导致肿瘤对多种传统化疗药物的耐药,如氟尿嘧啶类药物、去甲基化药物和铂类药物[24]。因此,对于治疗dMMR的晚期和复发性子宫内膜样腺癌患者是一项重大的挑战,临床迫切需要新的有效的治疗手段。辅助放疗在MMR蛋白表达缺失的子宫内膜癌中发挥更重要的作用,如Franchitto等[25]发表的MSH2缺陷细胞可能对辐射的敏感性有所增加。同样,Reijnen等[26]研究显示,辅助放疗可提高dMMR患者的特异性生存率。dMMR的肿瘤患者表现为高水平的突变,导致MSI[27]。突变增加通常表现为新抗原,招募并激活宿主免疫细胞[28]。有研究[29]表明服用阿司匹林能够降低结直肠癌及子宫内膜癌的发病风险。研究[30]表明,肿瘤可通过某些免疫检查点途径以达到免疫抵抗,免疫检查点多数是由受体–配体作用而启动的,例如肿瘤通过上调细胞程序性死亡-配体1(programmed cell death 1 ligand 1,PD-L1),PD-L1和T细胞上的程序性死亡受体1(programmed cell death protein 1,PD-1)相互作用,从而抑制活化的T细胞介导的肿瘤细胞死亡。因此,激活或增强抗肿瘤免疫反应最有效的免疫干预措施之一是通过使用抗体来阻断免疫检查点。
本研究收集515例子宫内膜样腺癌,采用IHC检测MMR蛋白表达情况,并且对MLH1表达缺失的标本进行MLH1基因甲基化检测,以初步筛查出LS患者,对dMMR相关患者的临床病理学特征进行探讨,并对筛选适合免疫治疗的患者提供依据。
利益冲突声明:所有作者均声明不存在利益冲突。
[参考文献]
[1] BELL D W, ELLENSON L H. Molecular genetics of endometrial carcinoma[J]. Annu Rev Pathol, 2019, 14: 339-367.
[2] LYNCH H T, LYNCH P M, LANSPA S J, et al. Review of the Lynch syndrome: history, molecular genetics, screening, differential diagnosis, and medicolegal ramifications[J]. Clin Genet, 2009, 76(1): 1-18.
[3] LU K H, SCHORGE J O, RODABAUGH K J, et al. Prospective determination of prevalence of lynch syndrome in young women with endometrial cancer[J]. J Clin Oncol, 2007, 25(33): 5158-5164.
[4] YAMAMOTO H, IMAI K. Microsatellite instability: an update[J]. Arch Toxicol, 2015, 89(6): 899-921.
[5] DE' ANGELIS GL, BOTTARELLI L, AZZONI C, et al. Microsatellite instability in colorectal cancer [J]. Acta Biomed, 2018, 89(9s): 97-101.
[6] SHIA, BLACK D, HUMMER A J, et al. Routinely assessed morphological features correlate with microsatellite instability status in endometrial cancer[J]. Hum Pathol, 2008, 39(1): 116-125.
[7] KWON J S, SUN C C, PETERSON S K, et al. Cost-effectiveness analysis of prevention strategies for gynecologic cancers in Lynch syndrome[J]. Cancer, 2008, 113(2): 326-335.
[8] CHAO X P, LI L, WU M, et al. Comparison of screening strategies for Lynch syndrome in patients with newly diagnosed endometrial cancer: a prospective cohort study in China[J]. Cancer Commun (Lond), 2019, 39(1): 42.
[9] SHENG J Q, FU L, SUN Z Q, et al. Mismatch repair gene mutations in Chinese HNPCC patients[J]. Cytogenet Genome Res, 2008, 122(1): 22-27.
[10] MANCHANA T, ARIYASRIWATANA C, TRIRATANACHAT S, et al. Lynch syndrome in Thai endometrial cancer patients[J]. Asian Pac J Cancer Prev, 2021, 22(5): 1477-1483.
[11] 晋 薇,王利群,刘 有 , 等. 子宫内膜癌组织中MMR蛋白表达及MLH1基因甲基化的临床意义[J]. 中华妇产科杂志, 2018, 53(12): 823-830.
JIN W, WANG L Q, LIU Y, et al. Expression and clinical significance of MMR protein and MLH1 promoter methylation testing in endometrial cancer[J]. Chin J Obstet Gynecol, 2018, 53(12): 823-830.
[12] ZHAO S S, CHEN L L, ZANG Y Q, et al. Endometrial cancer in Lynch syndrome[J]. Int J Cancer, 2022, 150(1): 7-17.
[13] RYAN N A J, MORRIS J, GREEN K, et al. Association of mismatch repair mutation with age at cancer onset in Lynch syndrome: implications for stratified surveillance strategies[J]. JAMA Oncol, 2017, 3(12): 1702-1706.
[14] BI R, TU X Y, XIAO Y X, et al. Clinicopathological analysis of the expression of mismatch repair protein in endometrial carcinoma[J]. Chin J Pathol, 2016, 45(5): 302-307.
[15] MCMEEKIN D S, TRITCHLER D L, COHN D E, et al. Clinicopathologic significance of mismatch repair defects in endometrial cancer: an NRG oncology/gynecologic oncology group study[J]. J Clin Oncol, 2016, 34(25): 3062-3068.
[16] WORKEL H H, KOMDEUR F L, WOUTERS M C, et al. CD103 defines intraepithelial CD8+ PD1+ tumour-infiltrating lymphocytes of prognostic significance in endometrial adenocarcinoma[J]. Eur J Cancer, 2016, 60: 1-11.
[17] SHIKAMA A, MINAGUCHI T, MATSUMOTO K, et al. Clinicopathologic implications of DNA mismatch repair status in endometrial carcinomas[J]. Gynecol Oncol, 2016, 140(2): 226-233.
[18] SIEGEL R L, MILLER K D, JEMAL A. Cancer statistics, 2015[J]. CA Cancer J Clin, 2015, 65(1): 5-29.
[19] HOANG L N, KINLOCH M A, LEO J M, et al. Interobserver agreement in endometrial carcinoma histotype diagnosis varies depending on the Cancer Genome Atlas (TCGA)-based molecular subgroup[J]. Am J Surg Pathol, 2017, 41(2): 245-252.
[20] LEÓN-CASTILLO A, DE BOER S M, POWELL M E, et al. Molecular classification of the PORTEC-3 trial for highrisk endometrial cancer: impact on prognosis and benefit from adjuvant therapy[J]. J Clin Oncol, 2020, 38(29): 3388-3397.
[21] WILLIAMS A B, SCHUMACHER B. p53 in the DNA-damagerepair process[J]. Cold Spring Harb Perspect Med, 2016, 6(5): a026070.
[22] CRANSTON A, BOCKER T, REITMAIR A, et al. Female embryonic lethality in mice nullizygous for both MSH2 and p53[J]. Nat Genet, 1997, 17(1): 114-118.
[23] SUBRAMANIAN D, GRIFFITH J D. Modulation of p53 binding to holliday junctions and 3-cytosine bulges by phosphorylation events[J]. Biochemistry, 2005, 44(7): 2536-2544.
[24] GUILLOTIN D, MARTIN S A. Exploiting DNA mismatch repair deficiency as a therapeutic strategy[J]. Exp Cell Res, 2014, 329(1): 110-115.
[25] FRANCHITTO A, PICHIERRI P, PIERGENTILI R, et al. The mammalian mismatch repair protein MSH2 is required for correct MRE11 and RAD51 relocalization and for efficient cell cycle arrest induced by ionizing radiation in G2 phase[J]. Oncogene, 2003, 22(14): 2110-2120.
[26] REIJNEN C, KÜSTERS-VANDEVELDE H V N, PRINSEN C F, et al. Mismatch repair deficiency as a predictive marker for response to adjuvant radiotherapy in endometrial cancer[J]. Gynecol Oncol, 2019, 154(1): 124-130.
[27] LYNCH H T, SNYDER C L, SHAW T G, et al. Milestones of lynch syndrome: 1895-2015[J]. Nat Rev Cancer, 2015, 15(3): 181-194.
[28] KLOOR M, BECKER C, BENNER A, et al. Immunoselective pressure and human leukocyte antigen class Ⅰ antigen machinery defects in microsatellite unstable colorectal cancers[J]. Cancer Res, 2005, 65(14): 6418-6424.
[29] BURN J, BISHOP D T, MECKLIN J P, et al. Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome[J]. N Engl J Med, 2008, 359(24): 2567-2578.
[30] PARDOLL D M. The blockade of immune checkpoints in cancer immunotherapy[J]. Nat Rev Cancer, 2012, 12(4): 252-264.


