【论著】| 伴MYC、BCL2、BCL6基因重排的DLBCL/HGBL临床病理学特征分析
时间:2023-10-12 14:24:53 热度:37.1℃ 作者:网络
[摘要] 背景与目的:伴MYC、BCL2和BCL6基因重排的弥漫性大B细胞淋巴瘤/高级别B细胞淋巴瘤(diffuse large B-cell lymphoma/high-grade B-cell lymphoma,DLBCL/HGBL)又称三重打击淋巴瘤(triple-hit lymphoma,THL),其发病率低且文献报道较少,人们对其缺乏充分认识。本研究旨在探讨THL的临床病理学特征及患者预后。方法:收集复旦大学附属肿瘤医院病理科2016年6月—2021年12月诊断的THL病例10例,回顾性分析其临床特征,采用H-E染色观察其组织病理学特征,采用免疫组织化学法分析其免疫表型,采用荧光原位杂交(fluorescence in situ hybridization,FISH)法检测MYC、BCL2和BCL6基因重排,采用EB病毒编码RNA(Epstein-Barr virus-encoded RNA,EBER)原位杂交法检测判断EB病毒的感染状态。结果:10例THL患者中,男性4例,女性6例。中位年龄54岁(43~80岁)。其中2例发生在淋巴结,6例发生在结外器官,其余2例结内外均受累。临床分期Ⅲ/Ⅳ期4例(40%),Ⅰ/Ⅱ期6例(60%)。40%(4/10)的患者国际预后指数(international prognostic index,IPI)评分≥3分。50%(4/8)的患者有骨髓侵犯。2例(20%)有B症状。40%(4/10)的患者有乙肝病毒既往感染史。显微镜下观察5例呈非特指DLBCL(DLBCL, not otherwise specified,DLBCL-NOS)形态,2例兼具DLBCL与伯基特淋巴瘤特征,1例呈母细胞样形态,其余2例因组织挤压严重无法准确分类。免疫组织化学染色显示,80%为生发中心B细胞(germinal center B-cell,GCB)型,20%为非GCB(non-GCB)型;78%(7/9)为MYC/BCL2双表达,BCL6阳性率为80%,Ki-67增殖指数均≥80%。FISH检测显示,10例均同时有MYC、BCL2和BCL6基因重排。EBER原位杂交均呈阴性。除1例手术切除病灶后未化疗外,9例均接受系统治疗。10例患者的总生存期为2.0~55.5个月,中位总生存期为16.8个月。1年总生存率为68.6%,其中Ⅰ/Ⅱ期患者的1年总生存率100%,Ⅲ/Ⅳ期患者为25%。结论:THL好发于中老年人,以结外器官受累更常见,是一组形态学表现多样、以GCB型为主并常伴有MYC/BCL2双表达的侵袭性B细胞淋巴瘤。本研究患者中临床分期Ⅰ/Ⅱ期占多数且预后较好,因此及早甄别THL对于及时干预、改善预后具有重要临床意义。
[关键词] 弥漫性大B细胞淋巴瘤/高级别B细胞淋巴瘤;三重打击淋巴瘤;基因重排;临床病理学特征;免疫表型;生存
[Abstract] Background and purpose: Diffuse large B-cell lymphoma/high-grade B-cell lymphoma (DLBCL/HGBL) with gene rearrangement of MYC, BCL2 and BCL6, also known as triple-hit lymphoma (THL), has a low incidence and relevant literature is limited. Thus comprehensive and sufficient understanding is lacking. The purpose of this study was to explore the clinicopathological features and prognosis of this rare disease. Methods: Ten cases of THL diagnosed in Department of Pathology, Fudan University Shanghai Cancer Center from June 2016 to December 2021 were collected. Clinical features were analyzed retrospectively. Histopathological features were observed using H-E stain. Immunophenotype was analyzed by immunohistochemistry. The rearrangement of MYC, BCL2 and BCL6 genes was detected by fluorescence in situ hybridization (FISH), and Epstein-Barr virus (EBV) infection was detected by in situ hybridization using EBV-encoded RNA (EBER). Results: Of the 10 cases, 4 cases were male and 6 cases were female. The median age was 54 years (43-80 years). Two cases occurred in lymph nodes, 6 cases involved extranodal organs, and both lymph nodes and extranodal organs were involved in the other 2 cases. There were 4 cases (40%) with clinical stage Ⅲ/Ⅳ disease and 6 cases (60%) with clinical stage Ⅰ/Ⅱ disease. 40% (4/10) patients had international prognostic index (IPI) score ≥3. 50% (4/8) patients had bone marrow invasion. Two (20%) cases had B symptoms. 40% (4/10) patients had a history of hepatitis B virus infection. Five cases had the morphology of DLBCL, not otherwise specified (DLBCL-NOS); Two cases showed morphological features intermediate both DLBCL and Burkitt lymphoma; One case had a blastoid cytomorphology, and the other 2 cases failed to be classified accurately because of serious crushing artifacts of the tissue. Immunophenotypically, 80% of the cases were of germinal center B-cell (GCB) type and 20% were of non-GCB type. MYC/BCL2 double expression accounted for 78% (7/9), BCL6 positivity was found in 80% of the total cases, and the Ki-67 proliferation index was ≥80% in all cases. FISH showed that all 10 cases had MYC, BCL2 and BCL6 gene translocation rearrangement. EBV infection was consistently absent. All except one case received systemic treatment. The overall survival was 2.0-55.5 months (median, 16.8 months), and 1-year overall survival rate was 68.6%. The 1-year overall survival rates of patients with stage Ⅰ/Ⅱ disease and stage Ⅲ/Ⅳ disease were 100% and 25% respectively. Conclusion: THL mainly affects middle-aged and elderly patients, which occured more frequently in extranodal organs, and it is characterized by GCB immunophenotype and MYC/BCL2 double expression. A considerable number of patients have a clinical stage of Ⅰ/Ⅱ disease and a better prognosis in the current series, indicating that early identification of THL is of great importance for timely intervention and improving the prognosis.
[Key words] Diffuse large B-cell lymphoma/high-grade B-cell lymphoma; Triple-hit lymphoma; Gene rearrangement; Clinicopathological features; Immunophenotype; Survive
2017版世界卫生组织(World Health Organization,WHO)淋巴造血组织肿瘤分类标准[1]首次提出伴MYC、BCL2和(或)BCL6重排的高级别B细胞淋巴瘤(high-grade B-cell lymphoma,HGBL),即双重打击淋巴瘤(double-hit lymphoma,DHL)和三重打击淋巴瘤(triple-hit lymphoma,THL)的概念。2022年第5版WHO淋巴造血组织肿瘤分类标准[2]中不再强调BCL6基因重排,将伴有MYC与BCL2基因断裂重排、无论是否有BCL6基因重排的HGBL均归类为伴MYC和BCL2重排的弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL) /HGBL。既往研究[3-7]认为同时伴MYC、BCL2和BCL6重排的DLBCL/HGBL(即THL)具有侵袭性高、易复发及预后不良等特征。然而目前关于THL的文献报道较少,且多为不足10例的小样本及个案报道[8-16],因此对于这种少见疾病仍缺乏充分认识。尽管新版WHO淋巴造血组织肿瘤分类标准中不再强调THL的概念,但实际仍存在争议。因此增加对这组疾病临床特点、病理学特征、免疫表型及预后等的深入了解,有望为其精准诊断、准确分类及优化治疗策略提供更充分的依据。
1 材料和方法
1.1 临床资料
收集复旦大学附属肿瘤医院病理科2016年6月—2021年12月诊断的THL病例10例。所有病例均由2名经验丰富的淋巴造血组织病理专科医师复阅切片。通过查阅电子病例及电话随访获得临床资料及预后信息。
1.2 免疫组织化学检测
所有标本均经3.7%中性甲醛溶液固定,常规脱水,石蜡包埋,3~4 μm连续切片,H-E染色观察其组织病理学形态,使用Ventana Benchmark XT全自动免疫组织化学分析仪(美国Roche Ventana公司)进行EnVision二步法免疫组织化学染色。一抗包括CD20、BCL2、CD5、CD30、Ki-67、cyclin D1(以上均购自美国Roche公司)、CD10(福州迈新生物技术开发有限公司)、BCL6(德国Leica公司)、MYC(英国Abcam公司)、MUM1及P53(丹麦Dako公司)等。依据Hans分型法则[14]进行细胞起源分型。依据WHO分类[1]中的定义,将肿瘤细胞MYC蛋白表达≥40%且BCL2蛋白表达≥50%定义为双表达。
1.3 荧光原位杂交(fluorescence in situ hybridization,FISH)检测
应用MYC、BCL2、BCL6双色荧光分离探针试剂盒(购自美国Abbott公司)进行FISH检测,具体操作程序参照说明书进行。在荧光显微镜下计数至少100个有红、绿双色信号的细胞核。若肿瘤细胞内出现红、绿分离信号或单独红色、绿色信号时视为阳性细胞。当阳性细胞数占比≥15%时诊断为有该基因相关易位。肿瘤细胞显示3个及以上红、绿信号或红、绿融合的黄色信号时提示基因扩增。
1.4 EB病毒编码RNA(Epstein-Barr virus-encoded RNA,EBER)原位杂交检测
EBER探针购自德国Leica公司。按照试剂盒说明书进行EBER原位杂交检测。采用3,3-二氨基联苯胺(3,3-diaminobenzidine,DAB)显色方法,阳性信号着色为棕褐色。
2 结 果
2.1 临床特征
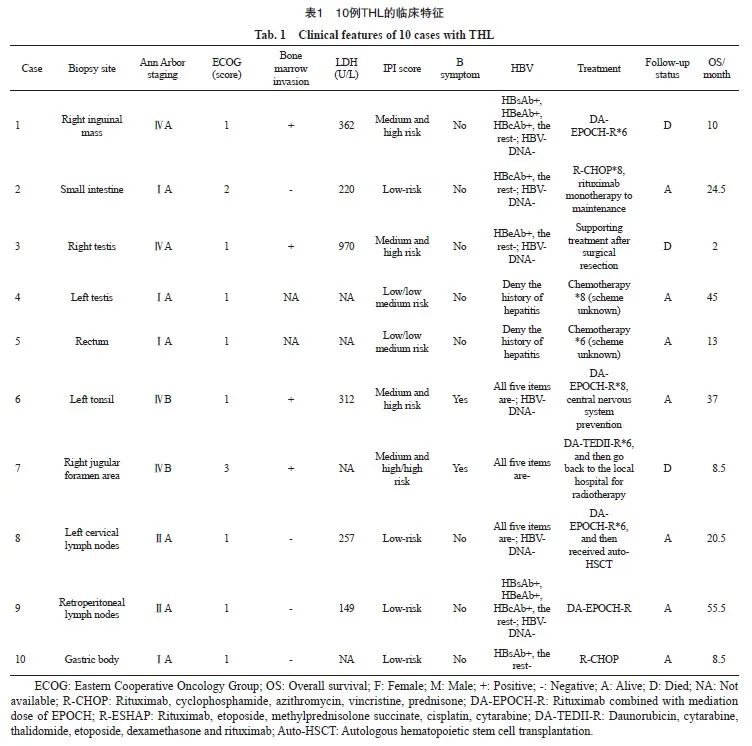
复旦大学附属肿瘤医院病理科2016年6月—2021年12月行MYC、BCL2、BCL6基因易位检测的侵袭性B细胞非霍奇金淋巴瘤(non-Hodgkin’s lymphoma,NHL)共924例,其中10例为THL,仅占1.1%。10例THL患者中,男性4例,女性6例。中位年龄54岁(43~80岁)。其中2例发生于淋巴结,6例发生于淋巴结外器官(2例发生于双侧睾丸,3例发生于胃肠道,1例表现为多发骨病变),其余2例表现为结内和结外多部位受累。6例患者临床分期为Ⅰ/Ⅱ期(60%),4例为Ⅲ/Ⅳ期(40%)。10例患者中2例(20%)有B症状(发热和体重下降各1例)。50%(3/6)患者乳酸脱氢酶(lactate dehydrogenase,LDH)水平高于正常值。国际预后指数(international prognostic index,IPI)评分中高危及高危(≥3分)占40%(4/10),低危及低中危(0~2分)占60%(6/10)。50%(4/8)的患者有骨髓侵犯。8例进行过乙肝5项检测:即乙肝病毒表面抗原(hepatitis B virus surface antigen,HBsAg)、乙肝病毒表面抗体(hepatitis B virus surface antibody,HBsAb)、乙肝病毒e抗原(hepatitis B virus e antigen,HBeAg)、乙肝病毒e抗体(hepatitis B virus e antibody,HBeAb)和乙肝病毒核心抗体(hepatitis B virus core antibody,HBcAb)。8例患者HBsAg和HBeAg均阴性,其中2例HBsAb、HBeAb、HBcAb三项抗体均阳性,各有1例分别HBcAb、HBeAb、HBsAb阳性,3例乙肝5项均阴性;其中6例进行过乙肝病毒(hepatitis B virus,HBV)DNA检测者均阴性。其余2例否认有乙型肝炎病史但未获得相关检测信息。具体临床特征见表1。
2.2 病理学形态特征
显微镜下观察患者的组织学形态,除2例因组织挤压严重无法进行准确的组织学分类外,5例(62.5%)患者呈非特指DLBCL(DLBCL, not otherwise specified,DLBCL-NOS)形态(图1A,图2A):肿瘤细胞核中等偏大,卵圆形或不规则,部分呈空泡状,核仁明显;细胞质中等量呈弱嗜碱性,间质中可见纤细的纤维胶原穿插分隔,其中1例伴有星空现象。2例(25%)患者肿瘤细胞形态兼具DLBCL和伯基特淋巴瘤(Burkitt lymphoma,BL)的特征(图1B):肿瘤细胞中等大小,细胞核圆形或卵圆形且染色质细,少量嗜碱性细胞质,核分裂象多见,细胞凋亡及坏死明显,并可见星空现象;背景中小淋巴细胞少见。1例(12.5%)为淋巴母细胞样形态(图1C):肿瘤细胞形态较单一,细胞核中等大小,染色质呈细颗粒状,核仁不明显,细胞质稀少;细胞排列密集,间质成分稀少,星空现象不明显。
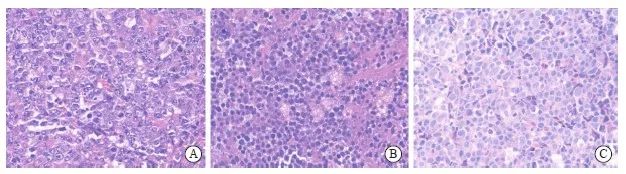
图1 THL的组织学形态
Fig.1 Histological features of THL
A: Histological morphology is DLBCL-like (H-E stain, ×400), with vacuolar nuclei and prominent nucleoli; B: This case showed morphological features intermediate both DLBCL and BL (H-E stain, ×400), composing of medium-sized tumor cells with starry-sky appearance; C: This THL case had a blastoid cytomorphology (H-E stain, ×400), the neoplastic cells are monotonous, with inconspicuous nucleoli and overlapping nuclei.
2.3 免疫表型及原位杂交结果
免疫组织化学染色及EBER原位杂交结果见表2,10例患者均弥漫表达成熟B细胞标志物CD20(图2B)。CD10、BCL6和MUM1阳性率分别为70%(7/10)、80%(8/10)和10%(1/10)(图2C~2E)。根据Hans分型法则,8例(80%)患者为生发中心B细胞(germinal center B-cell,GCB)型,2例(20%)为非GCB(non-GCB)型。MYC蛋白阳性率为89%(8/9),其中3例为40%~70%,5例≥70%(图2F)。BCL2阳性率为90%(9/10,图2G)。78%(7/9)的患者呈MYC/BCL2双表达,BCL6阳性率为80%,Ki-67增殖指数均较高(≥80%,图2H)。EBER原位杂交结果均阴性(0/6)。

图2 1例发生于睾丸的THL(病例4)组织学形态及免疫表型,免疫组织化学染色显示为GCB型且伴MYC/BCL2双表达
Fig. 2 A representative case of THL occurred in testis (case 4), immunohistochemical staining indicated GCB subtype with MYC/BCL2 double expression
A: Histological morphology is DLBCL-like (H-E stain, ×200); B: The tumor cells were strongly positive for CD20 staining (EnVision stain, ×200); C-E: The tumor cells were positive for CD10 and BCL6 and negative for MUM1 (EnVision stain, ×200), indicating a GCB type; F-G: Both MYC and BCL2 were positive, indicating its double expression status (EnVision stain, ×200); H: The Ki-67 proliferation index was as high as 95%(EnVision stain, ×200).

2.4 FISH检测结果
采用FISH分别检测MYC、BCL2及BCL6基因断裂重排,所有病例均有>50%的肿瘤细胞内可见红、绿分离信号,即均有MYC、BCL2和BCL6基因相关易位(图3A~3C)。其中1例患者(病例1)同时显示部分肿瘤细胞内MYC基因拷贝数增加,提示基因扩增(图3D)。
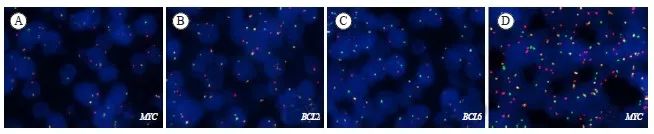
图3 FISH检测显示MYC、BCL2和BCL6基因异常
Fig. 3 FISH test showed alterations of MYC, BCL2 and BCL6 genes
A, B, C: The rearrangements of MYC, BCL2 and BCL6 were observed by FISH; D: MYC gene amplification was also identified in case 1.
2.5 治疗和预后
本组患者中4例行肿瘤切除术,其余6例均通过活检获得诊断。除1例手术切除病灶后因身体状况差仅行支持治疗外,其余9例均接受系统治疗。4例采用DA-EPOCH-R方案,其中1例完全缓解(complete response,CR)后接受自体造血干细胞移植(autologous hematopoietic stem cell transplantation,auto-HSCT);2例采用R-CHOP方案;1例采用DA-TEDII-R方案6个疗程后患者一般状况不佳回当地医院接受放疗;其余2例具体化疗方案不详。
本组患者截至随访结束7例存活,3例死亡。患者总生存期(overall survival,OS)为2.0~55.5个月,中位OS为16.8个月,1年OS率为68.6%。6例Ⅰ/Ⅱ期患者均存活,而4例Ⅲ/Ⅳ期患者仅1例存活,1年OS率分别为100%和25%。4例伴骨髓侵犯的患者中仅1例存活,1年OS率为25%;4例未累及骨髓的患者均存活,1年OS率为100%。4例有既往HBV感染史的患者中2例存活,1年OS率为50%;6例无HBV感染史的患者中5例存活,1年OS率为83.3%。
3 讨 论
THL较罕见,仅占DLBCL的0.4%[15]。目前国内外相关研究报道[8-11]较少,对该疾病的临床病理学特征及患者预后尚缺乏充分认识。尽管2022年新版WHO分类[2]不再强调BCL6基因断裂重排,并且不再强调THL这一概念,但实际上仍存在争议。因此,增加对这组特殊病例临床病理学特征的认识,对于准确诊断、合理分类、优化治疗策略及预后预测都具有重要意义。
THL好发于中老年人,本研究患者的中位年龄(54岁)与既往报道(51~64岁)[13,16- 17]相似。Huang等[16]报道40例THL患者中男性多于女性(5∶3),本研究并未显示出男女差异。THL好发于淋巴结外器官,如胃肠道、睾丸等,且易发生骨髓侵犯。THL侵犯罕见部位也有个别报道,如海绵窦、心包等[18-19]。值得注意的是,与既往文献中THL/DHL以Ⅲ/Ⅳ期为主(80%~90%)[6,9,16]不同,本研究患者中一半以上为Ⅰ/Ⅱ期,而Ⅲ/Ⅳ期占比较低(40%);高IPI评分患者的比例(40%≥3分)也低于既往报道(80%≥3分)。可能是由于本研究患者数较少,有待于积累更多病例以增加对其临床特征的充分认识。
有研究[20-22]表明,HBV感染与NHL密切相关,无论处于慢性HBV感染期还是既往感染过HBV的患者发生NHL的风险均有所增加,伴HBV感染的NHL患者比未感染过HBV的患者发病年龄更年轻且预后更差。Ren等[23]研究显示,与HBsAg阴性DLBCL(28%)相比,HBsAg阳性DLBCL(57%)患者呈现出更高频的BCL6基因易位重排。Zhang等[17]研究显示,THL/DHL患者中约53.2%伴既往HBV感染(其中包含3例THL患者且均有HBV感染),这部分患者的OS显著差于无HBV感染者,并且HBsAg+与MYC/BCL6-DHL及THL的发生有关。因此针对HBV感染的免疫调节方案可能会提高这部分患者常规放化疗和HSCT的治疗效果[24]。本研究中40%患者有HBV既往感染史,且其1年OS率较无HBV感染者低。但由于目前病例数有限,尚需积累更多病例进一步验证,并深入研究其机制,以探讨针对这部分患者的有效治疗策略。
THL/DHL的组织形态学表现多样,其中超过半数呈现出DLBCL-NOS的形态特征,介于DLBCL和BL之间者次之,母细胞样形态者较少[1,9]。免疫表型方面,64%~100%的THL为GCB型[25-27]。THL/DHL往往伴有MYC/BCL2蛋白双表达(70%~90%),且其阳性率显著高于DLBCL-NOS[13,17,27]。BCL6蛋白在THL/DHL中也具有较高的表达率(75%~90%),Ki-67增殖指数通常较高(>80%)[1]。因此有学者建议用上述蛋白表达作为THL的初筛手段,但由于THL缺乏特征性病理学形态特点并且免疫表型也缺乏特异性,因此依据组织学形态与免疫表型筛选THL并不准确且存在争议。基于此,WHO分类建议对所有DLBCL通过FISH检测以明确是否存在MYC、BCL2和BCL6基因重排[1]。但FISH检测费用昂贵,且在资源贫乏地区无法实现常规检测,因此是否针对所有DLBCL患者进行上述3个基因断裂重排的FISH检测目前并未达成共识。有学者建议对免疫表型GCB型且MYC/BCL2蛋白高表达的DLBCL/HGBL首先进行MYC基因重排检测,阳性者再进行BCL2和BCL6基因重排检测[26-28]。近年来Ziepert等[29]提出将MYC蛋白表达的临界值提高到70%,以此筛选出的MYC蛋白阳性病例中有44%通过FISH检测存在MYC基因重排,而MYC蛋白表达40%~70%的病例中仅11%存在MYC基因重排,提示70%作为MYC阳性的临界值可以更好地提示MYC基因重排。本研究患者中MYC蛋白表达≥70%者(56%)多于40%~70%者(33%),同样提示MYC蛋白表达 ≥70%与MYC重排具有更高的匹配度。
THL的一线治疗策略目前尚缺乏共识。由于THL存在MYC基因重排,因此对R-CHOP方案的敏感性欠佳[30-32]。Oki等[6]研究显示,接受强化诱导方案(DA-EPOCH-R、R-Hyper-CAVD)的DHL患者预后优于传统R-CHOP方案治疗者。另外一项回顾性研究[4]显示,THL/DHL患者接受强化诱导方案可以显著地延长中位无进展生存时间(progression-free survival,PFS)(21.6个月 vs 7.8个月),但不能改善患者的OS。本研究一线采用DA-EPOCH-R方案的4例患者中3例获得CR,1例部分缓解(partial response,PR)且在诊断10个月后死亡;采用R-CHOP方案的2例患者均获得CR。但由于病例数少且临床分期不同,尚不足以对不同治疗策略的疗效进行统计学分析。Auto-HSCT是治疗复发难治性NHL的有效手段[19,33],但是否可以改善THL患者的疗效和生存目前相关研究有限。有研究[34]显示,强化诱导方案化疗后采用BEAC(卡莫司汀、依托泊苷、阿糖胞苷和环磷酰胺)预处理方案联合组蛋白去乙酰化酶抑制剂西达本胺和大剂量利妥昔单抗,然后再进行auto-HSCT治疗,可以提高疗效及耐受性;但该研究纳入的病例数有限,因此仍需积累更多病例来进一步验证。综上所述,THL目前尚无规范化治疗策略,尤其复发难治性THL的治疗仍存在很大挑战,需要更多前瞻性临床试验进行探索。
目前普遍认为,THL患者预后较差,总体与DHL相似,中位OS较DLBCL-NOS差[10, 31, 35],但文献报道中的THL生存时间存在较大差异。Tomita等[10]报道的THL患者中位OS为4~6个月,而Huang等[16]报道的40例THL患者中位OS为18个月,1年OS率为61%。本研究结果与Huang等报道的结果相似。有学者[3,20]认为,临床分期晚、LDH水平在正常值3倍以上、伴骨髓或中枢神经系统侵犯者预后更差。本研究截至随访结束时Ⅰ/Ⅱ期患者均获得CR,1年OS率为100%,而Ⅲ/Ⅳ期患者的1年OS率仅为25%;尽管本组病例因数量有限尚不足以进行统计学分析,但目前结果提示早期准确诊断、及时干预对于改善THL患者的预后有重要意义,但尚需积累更大样本量并延长随访时间以进一步分析其生存及预后。有研究[36]显示,MYC拷贝数增加的THL/DHL患者(其中THL为3例)PFS和OS更差,但也有研究[37]显示,MYC拷贝数增加(其中THL为3例)与预后无关。本研究中1例MYC拷贝数增加的患者预后也较差。另外有研究认为,MYC重排伙伴基因为免疫球蛋白(Immunoglobulin,IG)基因的患者预后更差[29],而非IG者预后较好[38]。但也有研究[25]显示,MYC易位伙伴基因是否为IG对DHL/THL预后并无影响。鉴于THL病例数少且研究结论各异,因此需要更大样本量的研究以进一步探讨MYC基因拷贝数增加及与不同伙伴基因易位重排的临床病理学相关性及预后预测价值。
综上所述,THL好发于中老年人,以结外器官受累更常见,是一组形态学表现多样、以GCB亚型为主且常伴有MYC/BCL2双表达的侵袭性B细胞淋巴瘤。临床Ⅲ/Ⅳ期者临床进展迅速、易侵犯骨髓且预后较差;临床分期Ⅰ/Ⅱ期者并不少见,系统治疗后可以获得较好的预后。由于THL发病率/检出率较低,目前认识仍有限,因此仍需积累更多病例以进一步认识其临床生物学特征,对于早期诊断、及早干预具有重要的临床意义。深入探讨其分子遗传学特征及与DHL的相关性,有助于优化分类分型,为合理治疗、预后预测奠定基础。
利益冲突声明:所有作者均声明不存在利益冲突。
[参考文献]
[1]SWERDLOW S H, CAMPO E, HARRIS N L, et al. World Health Organization classification of tumours of haematopoietic and lymphoid tissues[M]. Lyon: IARC Press, 2017.
[2]ALAGGIO R, AMADOR C, ANAGNOSTOPOULOS I, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms[J]. Leukemia, 2022, 36(7): 1720-1748.
[3]PETRICH A M, GANDHI M, JOVANOVIC B, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis[J]. Blood, 2014, 124(15): 2354-2361.
[4]SARKOZY C, TRAVERSE-GLEHEN A, COIFFIER B. Double-hit and double-protein-expression lymphomas: aggressive and refractory lymphomas[J]. Lancet Oncol, 2015, 16(15): e555-e567.
[5]HOWLETT C, SNEDECOR S J, LANDSBURG D J, et al. Front-line, dose-escalated immunochemotherapy is associated with a significant progression-free survival advantage in patients with double-hit lymphomas: a systematic review and meta-analysis[J]. Br J Haematol, 2015, 170(4): 504-514.
[6]OKI Y, NOORANI M, LIN P, et al. Double hit lymphoma: the MD Anderson Cancer Center clinical experience[J]. Br J Haematol, 2014, 166(6): 891-901.
[7]ROSENTHAL A, YOUNES A. High grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6: double hit and triple hit lymphomas and double expressing lymphoma[J]. Blood Rev, 2017, 31(2): 37-42.
[8]PEMMARAJU N, GILL J, GUPTA S, et al. Triple-hit lymphoma[J]. Proc (Bayl Univ Med Cent), 2014, 27(2): 125-127.
[9]BACHER U, HAFERLACH T, ALPERMANN T, et al. Several lymphoma-specific genetic events in parallel can be found in mature B-cell neoplasms[J]. Genes Chromosomes Cancer, 2011, 50(1): 43-50.
[10]TOMITA N, TOKUNAKA M, NAKAMURA N, et al. Clinicopathological features of lymphoma/leukemia patients carrying both BCL2 and MYC translocations[J]. Haematologica, 2009, 94(7): 935-943.
[11]MOTLLÓ C, GRAU J, JUNCÀ J, et al. Translocation (3;8)(q27;q24) in two cases of triple hit lymphoma[J]. Cancer Genet Cytogenet, 2010, 203(2): 328-332.
[12]ELDESSOUKI T, HANLEY K, HAMADEH F, et al. “Triple hit” lymphomas: a retrospective cytology case series of an uncommon high grade B-cell malignancy with C-MYC, BCL-2 and BCL-6 rearrangements[J]. Diagn Cytopathol, 2018, 46(9): 807-811.
[13]WANG W, HU S M, LU X Y, et al. Triple-hit B-cell lymphoma with MYC, BCL2, and BCL6 translocations/rearrangements: clinicopathologic features of 11 cases[J]. Am J Surg Pathol, 2015, 39(8): 1132-1139.
[14]HANS C P, WEISENBURGER D D, GREINER T C, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray[J]. Blood, 2004, 103(1): 275-282.
[15]李 敏, 张秋露, 赵 炜, 等. 伴MYC、BCL2和(或)BCL6重排的高级别B细胞淋巴瘤在弥漫大B细胞淋巴瘤中的发生率[J]. 中华血液学杂志, 2021, 42(2): 124-128.
LI M, ZHANG Q L, ZHAO W, et al. Incidence of high-grade B-cell lymphoma with MYC, BCL2, and/or BCL6 rearrangements in diffuse large B-cell lymphoma[J]. Chin J Hematol, 2021, 42(2): 124-128.
[16]HUANG W T, MEDEIROS L J, LIN P, et al. MYC/BCL2/BCL6 triple hit lymphoma: a study of 40 patients with a comparison to MYC/BCL2 and MYC/BCL6 double hit lymphomas[J]. Mod Pathol, 2018, 31(9): 1470-1478.
[17]ZHANG J J, WENG Z P, HUANG Y H, et al. High-grade B-cell lymphoma with MYC, BCL2, and/or BCL6 translocations/rearrangements: clinicopathologic features of 51 cases in a single institution of South China[J]. Am J Surg Pathol, 2020, 44(12): 1602-1611.
[18]TRAN J, VICKERS A, PONCE C P, et al. Triple-hit lymphoma of the cavernous sinus[J]. Can J Ophthalmol, 2019, 54(2): e61-e66.
[19]EFSTATHOPOULOU A, GHIELMINI M, ZUCCA E. MYC/BCL2/BCL6 triple hit lymphoma of the pericardium: a case report and review of the literature[J]. J Cancer Res Clin Oncol, 2020, 146(9): 2435-2438.
[20] ZHOU X, PAN H X, YANG P, et al. Both chronic HBV infection and naturally acquired HBV immunity confer increased risks of B-cell non-Hodgkin lymphoma[J]. BMC Cancer, 2019, 19(1): 477.
[21] ABE S K, INOUE M, SAWADA N, et al. Hepatitis B and C virus infection and risk of lymphoid malignancies: a populationbased cohort study (JPHC Study)[J]. Cancer Epidemiol, 2015, 39(4): 562-566.
[22] ENGELS E A, CHO E R, JEE S H. Hepatitis B virus infection and risk of non-Hodgkin lymphoma in South Korea: a cohort study[J]. Lancet Oncol, 2010, 11(9): 827-834.
[23] REN W, YE X, SU H, et al. Genetic landscape of hepatitis B virus-associated diffuse large B-cell lymphoma[J]. Blood, 2018;131(24): 2670-2681.
[24] DENG L J, SONG Y Q, YOUNG K H, et al. Hepatitis B virusassociated diffuse large B-cell lymphoma: unique clinical features, poor outcome, and hepatitis B surface antigen-driven origin[J]. Oncotarget, 2015, 6(28): 25061-25073.
[25] AUKEMA S M, KREUZ M, KOHLER C W, et al. Biological characterization of adult MYC-translocation-positive mature B-cell lymphomas other than molecular Burkitt lymphoma[J]. Haematologica, 2014, 99(4): 726-735.
[26] SWERDLOW S H. Diagnosis of ‘double hit’ diffuse large B-cell lymphoma and B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma: when and how, FISH versus IHC[J]. Hematology Am Soc Hematol Educ Program, 2014, 2014(1): 90-99.
[27] SCOTT D W, KING R L, STAIGER A M, et al. Highgrade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements with diffuse large B-cell lymphoma morphology[J]. Blood, 2018, 131(18): 2060-2064.
[28] PEDERSEN M Ø, GANG A O, POULSEN T S, et al. Doublehit BCL2/MYC translocations in a consecutive cohort of patients with large B-cell lymphoma-a single centre’s experience[J]. Eur J Haematol, 2012, 89(1): 63-71.
[29] ZIEPERT M, LAZZI S, SANTI R, et al. A 70% cut-off for MYC protein expression in diffuse large B-cell lymphoma identifies a high-risk group of patients[J]. Haematologica, 2020, 105(11): 2667-2670.
[30] CUCCUINI W, BRIERE J, MOUNIER N, et al. MYC+ diffuse large B-cell lymphoma is not salvaged by classical R-ICE or R-DHAP followed by BEAM plus autologous stem cell transplantation[J]. Blood, 2012, 119(20): 4619-4624.
[31] KÜHNL A, CUNNINGHAM D, COUNSELL N, et al. Outcome of elderly patients with diffuse large B-cell lymphoma treated with R-CHOP: results from the UK NCRI R-CHOP14V21 trial with combined analysis of molecular characteristics with the DSHNHL RICOVER-60 trial[J]. Ann Oncol, 2017, 28(7): 1540-1546.
[32] GREEN T M, YOUNG K H, VISCO C, et al. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone[J]. J Clin Oncol, 2012, 30(28): 3460-3467.
[33] GROSS T G, HALE G A, HE W S, et al. Hematopoietic stem cell transplantation for refractory or recurrent non-Hodgkin lymphoma in children and adolescents[J]. Biol Blood Marrow Transplant, 2010, 16(2): 223-230.
[34] KANG J N, ZHANG Y Z, DING S, et al. Modified conditioning regimen with chidamide and high-dose rituximab for triple-hit lymphoma[J]. J Cell Mol Med, 2021, 25(22): 10770-10773.
[35] SNUDERL M, KOLMAN O K, CHEN Y B, et al. B-cell ymphomas with concurrent IGH-BCL2 and MYC rearrangements are aggressive neoplasms with clinical and pathologic features distinct from Burkitt lymphoma and diffuse large B-cell lymphoma[J]. Am J Surg Pathol, 2010, 34(3): 327-340.
[36]VALERA A, LÓPEZ-GUILLERMO A, CARDESA-SALZMANN T, et al. MYC protein expression and genetic alterations have prognostic impact in patients with diffuse large B-cell lymphoma treated with immunochemotherapy[J]. Haematologica, 2013, 98(10): 1554-1562.
[37] TZANKOV A, XU-MONETTE Z Y, GERHARD M, et al. Rearrangements of MYC gene facilitate risk stratification in diffuse large B-cell lymphoma patients treated with rituximab- CHOP[J]. Mod Pathol, 2014, 27(7): 958-971.
[38] ADAMS T, FUCHS D, SHADOAN P K, et al. Unexpected favorable outcome in a patient with high grade B-cell lymphoma with abnormalities of MYC, BCL6 and BCL2 loci[J]. Cancer Genet, 2018, 222-223: 25-31.


